Episiotomy’s prevalence and its associated factors before and after the Brazilian Obstetrics Violence Law
Jan Pawel Andrade Pachnicki, M.D., Ph.Da,b,c,d*, Bruno Damasceno da Silvaa, Isadora Goetten Santos da Silvab
aDepartment of Obstetrics of Pontifical Catholic University of Paraná – R. Imaculada Conceição, 1155 - Prado Velho, Curitiba – PR / Brasil, 80215-901.
bDepartment of Gynecology of Mackenzie Evangelical Medical School of Paraná – R. Padre Anchieta, 2770 - Bigorrilho, Curitiba – PR / Brasil, 80730-000.
cDepartment of Tocogynecology of Federal University of Paraná – R. General Carneiro, 181 - Alto da Glória, Curitiba – PR / Brasil, 80060-900.
dDepartment of Gynecology and Obstetrics of Positivo University – Cidade Industrial de Curitiba, Curitiba – PR / Brasil, 81290-000.
*Corresponding author: Jan Pawel Andrade Pachnicki, M.D., Ph.D. Department of Obstetrics of Pontifical Catholic University of Paraná – R. Imaculada Conceição, 1155 - Prado Velho, Curitiba – PR / Brasil, 80215-901.
Received: 29 July 2025; Accepted: 11 August 2025; Published: 15 August 2025
Article Information
Citation: Jan Pawel Andrade Pachnicki, M.D., Ph.D, Bruno Damasceno da Silva, Isadora Goetten Santos da Silva. Episiotomy’s prevalence and its associated factors before and after the Brazilian Obstetrics Violence Law. Obstetrics and Gynecology Research. 8 (2025): 122-128.
View / Download Pdf Share at FacebookAbstract
Objective:
Understanding episiotomy’s prevalence before and after the implementation of Obstetrics Violence Law, in order to demonstrate the procedure’s role in preventing perineal lacerations and its influences on neonatal outcomes.
Methods:
The sample of this retrospective cross-sectional study consists in 5,412 patients undergoing vaginal delivery from 2016 to 2022 in a hospital located at the metropolitan region of Curitiba – PR. Data such as age, parity, episiotomy, perineal laceration, use of forceps and/or vacuum extractor, Apgar score were gathered, with the quantitative variables described by mean, standard deviation, median, minimum and maximum, and categorical variables by frequency and percentage. To assess the association between two categorical variables it was used the Chi-square test and Fisher’s exact test. Comparison between two odds ratio (OR) was performed using the Breslow-Day test and for the common estimate of two OR the Mantel-Haenzel approach. The Mann Whitney non-parametric test was used to compare cases with and without episiotomy, as to the Apgar values. Values of p<0.05 indicated statistical significance.
Results:
2,065 were primiparous and 3,347 were multiparous. The average age was 24.4 years-old. There was a reduction in the number of episiotomies after the brazilian law from 19.32% to 16.53% (p=0.011). There is a higher prevalence of episiotomies in primiparous patients OR=4.91 (95%CI: 4.26-5.65) and p<0.001 for both periods. Not performing episiotomy was seen to be a risk factor for perineal laceration OR=7.44 (95%CI: 5.60-9.88), p<0.001. In instrumented childbirth, episiotomy proved to be protective in both primiparous OR=0.098 95%CI (0.030 – 0.322), p<0.001 and multiparous patients OR=0.154 95%CI (0.031 – 0.759), p=0.04. Episiotomy was not related to better neonatal outcomes.
Conclusions:
There was a significant reduction in the prevalence of episiotomies after the Obstetric Violence Law. In addition, it was observed that a practice aimed at selective episiotomy seems to play an important role in preventing perineal lacerations.
Keywords
Episiotomy, Brazil, Epidemiology, Obstetric Violence
Episiotomy articles, Brazil articles, Epidemiology articles, Obstetric Violence articles.
Article Details
INTRODUCTION
Medicine is a science that evolves daily, and technology and research are always looking to improve this Science. Thus, evidence based medicine and progress must go together to transform and modernize old practices. Currently an Obstetrics topic has been widely debated: episiotomy as a routine practice in assistance to the vaginal delivery. Practice of performing intrapartum episiotomy has become a matter of discussion in Brazil mainly after the law No. 7,867, implemented at 2017, which talks about Obstetrics Violence [1].
The first report of episiotomy dates from 1742. This procedure was used by Felding Ould at Rotunda Hospital in Dublin and aimed to increase the vagina opening through an perineal incision during the 2nd period of childbirth, helping in difficult births. In 1851 Taliaferro introduced episiotomy in the United States of America and over time it became a routine practice in Obstetrics centers [2]. Posteriorly, another milestone of this procedure took place in the 20th century by DeLee, who defended the use of routine mediolateral episiotomy, and by Pomeroy who preferred median episiotomy as a way to avoid extensive perineal lacerations. As they were influential gynecologists at their time, this practice was expanding without scientific evidence about the risks and benefits of the routine procedure [3].
Given the worldwide use of episiotomy and thinking to answer the questions about the benefits and harms of using this procedure, in 2017, an update of Cochrane systematic review compared the routine use versus selective episiotomy and demonstrated that in practice an episiotomy is likely to mean a longer hospital stay, postnatal care and increasing health care costs. Accordingly, current evidence do not justify performing routine episiotomy as there is an increase in perineal injuries as well as there is no decrease in intrapartum bleeding, perineal infection, long-term dyspareunia and long-term urinary incontinence when compared to selective episiotomy [4,5]. Regarding postpartum pain, women who underwent episiotomy reported feeling less pain than patients who suffered some type of obstetrical injury of the anal sphincter. The use of Routine episiotomy as a way to prevent severe perineal trauma is questionable as many women undergo episiotomy without need in different parts of the world. Not all normal births end in perineal trauma and even in obstetric emergencies episiotomy may not reduce high-grade perineal injury [6].
To show how academic contribution and discussions about obstetric malpractice impact in medical interventions, the aims of this study were to know the prevalence of episiotomies before and after the implementation of Obstetric Violence Law in Brazil and what is its impact on the number of procedures performed in a hospital down the Metropolitan Region of Curitiba - Paraná. In addition, to demonstrate the role of episiotomy in preventing intrapartum perineal laceration and whether the practice of episiotomy interferes with Apgar score in the first and fifth minutes of the newborn.
Methods
This is a retrospective cross-sectional epidemiological study. Its data were collected from Hospital and Maternity Alto Maracanã which is located in the Curitiba’s Metropolitan Region, in Colombo / PR.
In data collection, 5,412 medical records of patients who underwent vaginal delivery between 2016 and 2022 were sought focusing information on whether or not an episiotomy was performed during intrapartum and if there was any type of perineal laceration / obstetrical lesion of the anal sphincter. These informations were tabulated in an Excel spreadsheet. It was also collected data about patient age, number of pregnancies, new born gestacional age by Parkin method, use of forceps, use of vacuum extractor, type of anesthesia used, date of delivery and newborn’s Apgar in the first and fifth minutes.
Inclusion criteria covered all patients who underwent vaginal delivery in the period of of the study. Consequently, all patients not undergoing vaginal delivery were excluded from the present research. The period of 2016 and 2017 was considered as before the Brazilian Obstetrics Violence Law and the subsequent years as after the law for further comparisons.
After this data collection, the mean age of patients was analyzed so as the prevalence of primiparous and multiparous patients before and after the implementation of the law. The authors annalyzed the prevalence of episiotomies performed in general, and also compared between primiparous and multiparous, before and after the study’s reference. Prevalence of perineal laceration in patients undergoing and not undergoing episiotomy, as well as whether the Apgar of the first and fifth minutes suffered significant changes by the procedure, was also noticed.
Quantitative variables were described as mean, standard deviation, median, minimum and maximum, and categorical variables as frequency and percentage. For assessing the association between two categorical variables the Chi-square Test and, in some cases, Fisher's Exact Test were used. The estimated measure of association was the odds ratio (OR) with respective 95% confidence intervals. The comparison between two odds ratios was made using the Breslow-Day Test and for the common estimate of two ORs the Mantel-Haenzel approach was used. The non-parametric Mann-Whitney Test was used to compare cases with and without episiotomy in terms of Apgar values (1’, 5’ and mean of 1’ and 5’). Values of p<0.05 indicated statistical significance. Data were analyzed with the computer program IBM SPSS Statistics v.20.0. Armonk, NY: IBM Corp.
This study was approved by the Ethics and Research Committee (CEP) of the Pontifical Catholic University of Paraná - PUCPR under the protocol CAAE 31480820.9.0000.0020.
Results
Between 2016 and 2022, 5412 medical records of pregnant patients in the Metropolitan Region of Curitiba / PR were annalyzed. 2065 (38.16%) were primiparous and 3347 (61.84%) were multiparous women. These patients were stratified into primiparous and multiparous before and after the obstetric violence law, as shown in table 1.
Table 1: Number of stratified patients before and after de Obstetrics Violence Law.
|
Period |
Primiparous |
Multiparous |
Total |
|
Before Law |
1332 |
2124 |
3456 |
|
38.54% |
61.46% |
||
|
After law |
733 |
1223 |
1956 |
|
37.42% |
62.52% |
||
|
Total |
2065 |
3347 |
5412 |
p=0.437. Chi-Square Test, p<0.05
Source: The Authors.
The mean age of patients throughout the annalyzed period was 24.4 years. The minimum age found was 12 years-old and the maximum 45 years-old; the standard deviation (SD) is 6.0. For primigravid women, the mean age found was 20.7 years-old (minimum aged in 12 years-old) and 26.6 for multigravids (maximum aged 40 years-old). In addition, the mean age of patients before and after the law was annalyzed, respectively: 24.2 and 24.7 years-old.
Table 2 portray the prevalence of episiotomies, without differentiating primiparae from multiparae, performed before and after the law. Of the 3452 patients found before the law, 667 underwent episiotomy, against 2785 who did not undergo the procedure. After the law, 324 patients underwent episiotomy and 1636 patients did not need this obstetric intervention.
Table 2: Episiotomies performed before and after the Brazilian Obstetrics Violence Law.
|
Period |
Episiotomy |
Total |
|
Before Law |
No Yes |
3452 |
|
2785 667 |
||
|
80.68% 19.32% |
||
|
After law |
1636 324 |
1960 |
|
83.47% 16.53% |
||
|
Total |
4421 991 |
5412 |
p=0.011. Chi-Square Test, p<0.05
Source: The Authors.
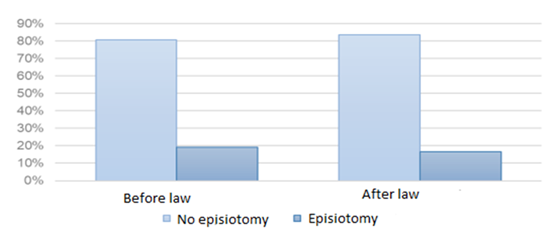
In the comparison between these two periods, a significant reduction (p=0.011) was found in the number of episiotomies after the obstetric violence law. Figure 1 depicts this 19.32% reduction in patients undergoing episiotomy to 16.53% after the implentation of the law.
Source: The Authors.
In addition, patients were separated into primiparous/multiparous and the prevalence of episiotomy before and after the law was calculated. In the 2016 and 2017 group, 1,332 primiparous were found of which 460 underwent episiotomy, and 2,124 multiparous of which 211 underwent episiotomy. The Odds Ratio (OR) found for this analysis was 4.78 with a 95% Confidence Interval (CI): 3.99 - 5.73, what showed that the chance of having an episiotomy, before the obstetric violence law for a primiparous patient is 4.78 times the chance of undergoing this procedure when compared to a multiparous patient. In the group from 2018 to 2022, 733 primiparous were found of which 224 underwent episiotomy and 1,223 multiparous of which 96 underwent the obstetric intervention. The OR found was 5.17 with 95%CI: 3.98 - 6.71, what showed that the chance of undergoing an episiotomy, after the obstetric violence law, for a primiparous patient is 5.17 times the chance of undergoing this procedure, when compared to a multiparous patient (table 3).
Table 3: Prevalence of Episiotomies in Primiparous and Multiparous before and after the Brazilian Obstetrics Violence Law.
|
Period |
Episiotomy |
Total |
|||
|
Yes |
No |
||||
|
Before Law |
460 |
872 |
1332 |
||
|
34.50% |
64.50% |
||||
|
Multiparous |
211 |
1913 |
2124 |
||
|
9.90% |
90.10% |
||||
|
Total |
671 |
2785 |
3456 |
||
|
Period |
|||||
|
Primiparous |
224 |
509 |
733 |
||
|
30.60% |
69.40% |
||||
|
Multiparous |
96 |
1127 |
1223 |
||
|
7.80% |
92.20% |
||||
|
Total |
320 |
1636 |
1956 |
||
p<0.001. Chi-Square Test, p<0.05
Source: The AuthorS.
For both periods, it was observed that there is a higher prevalence of episiotomies in primigravid patients compared to the multiparous group (p<0.001). In addition it was possible to establish a common OR for both periods estimated at 4.91 with 95% CI: 4.26 - 5.65. When comparing the periods before and after the law, in relation to the OR of the association between primiparous/multiparous and yes/no episiotomy no significant difference was found (p=0.634, Breslow-Day test).
As seen in table 4, there was a significant difference (p<0.001) between the number of patients who underwent episiotomy from those who didn’t regard perineal laceration. In this study, it was observed that not undergoing episiotomy behaved as a risk factor for perineal laceration revealing that the chance of suffering some degree of perineal laceration for a patient without episiotomy is 7.44 times the chance of laceration for a patient with episiotomy (OR=7,44 com IC95%: 5,60 - 9,88).
Table 4: Laceration’s prevalence in patients undergoing episiotomy
|
Episiotomy |
Laceration |
Total |
|
No |
Yes No |
|
|
1308 3113 |
4421 |
|
|
29.6% 70.4% |
||
|
Yes |
53 938 |
991 |
|
5.3% 94.7% |
||
|
Total |
1361 4051 |
5512 |
p<0,001. Chi-Square Test, p<0,05
Source: The Authors.
In addition, it was also possible to split the patients into non-instrumentalized deliveries and deliveries using forceps and/or vacum extractor. Of 1974 primiparous with non-instrumentalized deliveries, 611 underwent episiotomy of which 95.1% had none perineal laceration. On the other hand of 1363 patients without this intervention only 62.4% did not have any type of perineal tear (p<0.001). The group of multiparous women who underwent non-instrumentalized delivery had 3304 patients of which 278 were subject to episiotomy and 95.7% of these did not have perineal laceration, while 74.2% of patients who did not had episiotomy had the same outcome (p<0.001).
The Fischer’s Exact Test showed that there was significant association between episiotomy and laceration in primiparous (X2(1) = 18,099; p <0,001). The estimated OR was 0.098 with 95% CI (0.030-0.322) showing that, for this sample, selective episiotomy seems to be a protective fator for laceration in primigravidae in instrumental deliveries (vacum extractor and forceps). The same test showed yet that there was an association between episiotomy and laceration in multiparous (X2 (1) = 6,031; p = 0,04). The estimated OR was 0,154 IC95% (0,031 - 0,759) showing that selective episiotomy, even in women with more pregnancies, could be a protective factor for laceration.
In the present research, it was also possible to study neonatal outcomes from Apgar score according to tables 10 and 11. Data were annalyzed using nonparametric Mann-Whitney Test (p < 0.05) and it was evidenced how Apgar score behaves in the first and fifth minutes postpartum in relation to primigravid and multiparous women submitted or not to episiotomy. The fifth minute Apgar have significant diference in patients submitted or not to episiotomy (p=0,033). The average five minute Apgar score for patients without an episiotomy was 9.62 while the same parameter in patients with an episiotomy was 9.57. On the other hand the annalysis of the score in the first minute did not reveal a significant difference between the groups (p=0.337) as well as the mean obtained between the Apgar values in the first and fifth minute also did not showed statistical significance (p=0,096). Episiotomy, by the same way, was not associated with better neonatal outcome in multiparous women when we analyzes the Apgar score of the newborn in any moment: neither in first minute (p=0.127) nor in the fifth minute (p = 0.157), and not even between these two moments (p=0.82) – table 5.
Table 5: Apgar in primiparous and multiparous patients regarding episiotomy.
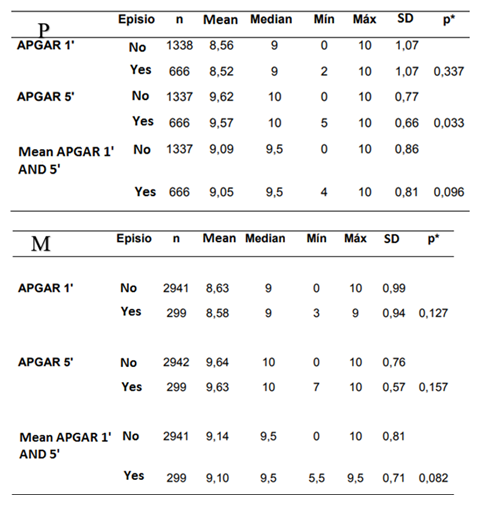
Nonparametric Mann-Whitney test (p < 0.05)
Source: The Authors.
Discussion
Episiotomy’s rate vary substantially between countries. For example, while in Taiwan the reports reach 100% of the vaginal deliveries, in Sweden this number reaches only 9.7%. In addition to this Scandinavian country, France and The Netherlands have also low rates (13.6% and 10.8%, respectively). That prevalence is closely linked to each country’s health policies. Countries like China and Argentina have high rates of episiotomy due to the routine use of this procedure for first birth, for example. However, there are places where this practice is no longer routine so the recorded number of this procedure are falling more and more such as in the USA and Israel; the first registered episiotomy’s rate of 60.9% in 1979 and only 24.5% in 2004, the second had a rate of 30% back at the 90’s and dropped to less than 5% in 2010 [5].
Brazil continues to decrease episiotomy’s rates: in 2000 there was a prevalence of approximately 94%, falling to 76% in 2006 and to 54% in 2014 [7]. This drop in Brazil numbers corroborates the data found in the present study since until the end of 2017 the rate of patients undergoing the procedure was 19.32%, while after that date it was only 16.53%. Although there was a general downfall, when its separeted into groups such as multiparous and primiparous, with or without episiotomy, there was none significant differece. This data suggest that there was already a reduction in routine episiotomies even before the law implementation.
Several studies suggest that the routine use of episiotomy has no benefit for pregnant women. A multicenter randomized trial showed that selectve episiotomy compared to routine episiotomy resulted in fewer mild perineal tears and also more intact perineum after delivery of multiparous women. It also recommended restrictive episiotomy policy to be established for all patients who will undergo uninstrumented vaginal delivery specially multiparous women [8]. Unfortunately this study could not compare routine and selective episiotomy since the sample only differentiates patients who underwent episiotomy and the ones that did not, and in addition the data did not measured perineal’s lacerations degree, only if there was or not a lesion. However, according to the annalysis of the presente research it was possible to observe that there was a significant reduction in lacerations of any degree in patients undergoing episiotomy. Despite the evidence supporting a selective practice of episiotomy use for deliveries that do not use forceps or vacum extractor, there are conflicting data when it comes to instrumental vaginal delivery.
There are reports that episiotomy has no effect on perineal damage as also reports of protective behavior for fourth degree tears... indeed, there are also reports of increased risck for third degree tears [9]. This study revealed a protective effect of episiotomy when it comes to tearing in instrumental deliveries. In addition, when the patients were analyzed globally without separating instrumental deliveries from spontaneous vaginal deliveries it was observed that episiotomy had a protective role in preventing lacerations.
A randomized clinical trial from 2017 analyzed the use of selective episiotomy versus a non-episiotomy protocol. It inclueded primigravid and multiparous patients and analysis were performed without stratification between parities. That was the first randomized clinical trial comparing the intention to never perform episiotomy with selective episiotomy, and it assigned 122 women to the selective episiotomy protocol versus 115 to the non-episiotomy protocol showing that when comparing the two groups in terms of perineal laceration there was no significant difference (p=0.86). The frequency of perineal laceration for selective episiotomy was 83.6% while for non-episiotomy it was 82.6%. Regarding this outcome the study questions wheter there is any indication for the use of the procedure even if selectively [10]. The data published in that study go against those found in this research since not performing any type of episiotomy behaved as a risk factor for perineal laceration.
In 2018, another clinical trial with 309 primiparous patients revealed that once again there was no significant difference between selective episiotomy versus no episiotomy when we talk about perineal laceration of any degree. Approximately 63% of the parturientes in the non-episiotomy protocol suffered perineal laceration while 65% who underwent selective episiotomy had the perineum injured [11]. As in the 2017 randomized clinical trial, the data published in the 2018’s study did not find a difference between groups diverging from the present study.
Another two cross sectional studies annalyzed vaginal deliveries without any type of obstetric intervention such as episiotomy, however there was no comparison with the selective use of episiotomy. These two studies suggested that it is possible to have a high prevalence of intact perineums without the use of episiotomy. In the Japanese study 49.5% of primiparous patients and 69.9% of multiparous did not have any type of laceration, in the global analysis (primiparous and multiparous) 64.2% off the patients had no perineal trauma [12]. In another observational study 58.7% of the patients remained with na intact perineum [13]
The present research also revealed a high percentage of patients without perineal laceration when they did not undergo episiotomy (62.4% of primiparous, 74% of multiparous, and 70.4% of patients in global analysis). However when compared to patients submitted to episiotomy the results obtained exceed 94% of all patients without perineum tearing which suggests episiotomy as a proctective factor. Based on this conflicting data found between this study and the literature it is proposed new randomized clinical trials with significant sample to clarify the issue.
Regardind neonatal outcomes represented in this study as the analysis of the Apgar score in the first and fifth minutes of life, studies showed that the use of episiotomy does not influence the condition of the newborn at birth. Negative outcomes were defined as admission to a Neonatal Intesive Care Unit or birth asphyxia which is represented by an Apgar score less than 7 both in primiparous or multiparous and for instrumental and non instrumental vaginal deliveries [8,9]. The data found in these studies are in line with those presented in the present sample. Although a significant difference is observed in the fifth minute Apgar only for primiparous patients, episiotomy is not associated with a better outcome.
Conclusion
Since it was shown a significant reduction in episiotomies’ prevalence in the population studied, the present study brought encouraging data in facing an old challenge: reducing obstetrics malpractice. Academic discussions and laws related to the theme played a significant role in this scenario change. In addition it was possible to observe that a practice focused on selective episiotomy seems to have an important role in preventing perineal lacerations, whether minor to more severe traumas such as anal sphincter laceration, acting as a proctective factor. In time, it was possible to demonstrate that neonatal outcomes were not influenced by episiotomy.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Mattar R, de Aquino MMA, Mesquita MRS. A prática da episiotomia no Brasil. Rev. Bras. Ginecol. Obstet Vol. 29 (2007): 1-2.
- Muhleman MA, Aly I, Walters A, et al. To cut or not to cut, that is the question: A review of the anatomy, the technique, risks, and benefits of an episiotomy. Clin Anat 30 (2017): 362-372.
- Corrêa Junior MD, Passini Júnior R. Selective Episiotomy: Indications, Techinique, and Association with Severe Perineal Lacerations. Rev Bras Ginecol Obstet 38 (2016): 301-307.
- Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev 1 (2009): CD000081.
- Jiang H, Qian X, Carroli G, et al. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database of Systematic Reviews 2 (2017): Art. No.: CD000081.
- Sultan AH, Thakar R, Ismail KM, et al. The role of mediolateral episiotomy during operative vaginal delivery. Eur J Obstet Gynecol Reprod Biol 240 (2019): 192-196.
- Cunha CMP, Katz L, Lemos A, et al. Knowledge, Attitude and Practice of Brazilian Obstetricians Regarding Episiotomy. Rev Bras Ginecol Obstet 41 (2019): 636-646.
- Sangkomkamhang U, Kongwattanakul K, Kietpeerakool C, et al. Restrictive versus routine episiotomy among Southeast Asian term pregnancies: a multicentre randomised controlled trial. BJOG 127 (2020): 397-403.
- Macleod M, Strachan B, Bahl R, et al. A prospective cohort study of maternal and neonatal morbidity in relation to use of episiotomy at operative vaginal delivery. BJOG 115 (2008): 1688-1694.
- Amorim MM, Coutinho IC, Melo I, et al. Selective episiotomy vs. implementation of a non-episiotomy protocol: a randomized clinical trial. Reprod Health 14 (2017): 55.
- Sagi-Dain L, Bahous R, Caspin O, et al. No episiotomy versus selective lateral/mediolateral episiotomy (EPITRIAL): an interim analysis. Int Urogynecol J 29 (2018): 415-423.
- Suto M, Takehara K, Misago C, et al. Prevalence of Perineal Lacerations in Women Giving Birth at Midwife-Led Birth Centers in Japan: A Retrospective Descriptive Study. J Midwifery Womens Health 60 (2015): 419-427.
- Albers LL, Sedler KD, Bedrick EJ, et al. Factors related to genital tract trauma in normal spontaneous vaginal births. Birth 33 (2006): 94-100.


 Impact Factor: * 3.2
Impact Factor: * 3.2 Acceptance Rate: 76.63%
Acceptance Rate: 76.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 