Eyelid Reconstruction Following Mohs Micrographic Surgery: Outcomes, Comparison of Techniques and Complications, an Asian Perspective
Daniel Yuxiang Chin1*, David Zhiwei Law1, Llewellyn Kuan-Ming Lee1
1National Healthcare Group Eye Institute, Tan Tock Seng Hospital, Singapore
*Corresponding author: Daniel Chin, National Healthcare Group Eye Institute, Tan Tock Seng Hospital, Singapore.
Received: 19 June 2025; Accepted: 26 June 2025; Published: 07 July 2025;
Article Information
Citation: Daniel Yuxiang Chin, David Zhiwei Law, Llewellyn Kuan-Ming Lee. Eyelid Reconstruction Following Mohs Micrographic Surgery: Outcomes, Comparison of Techniques and Complications, an Asian Perspective. Journal of Ophthalmology and Research. 8 (2025): 39-46.
DOI: 10.26502/fjor.2644-002400104
View / Download Pdf Share at FacebookAbstract
Purpose: To evaluate the surgical outcomes, complications, and recurrence rates in patients undergoing eyelid reconstruction following Mohs micrographic surgery. Methods: This single-institution retrospective study included 25 patients who underwent eyelid reconstruction after Mohs surgery between January 1, 2014, and December 31, 2022. Data on demographics, lesion characteristics, surgical techniques, and outcomes were analysed. Results: The mean patient age was 67.2 years (range: 49–89); 72% were male and 28% were female. Majority were Chinese (68%) and the rest comprised other races (32%). Lesion sizes were classified as small (<20 mm, 36%), medium (20–30 mm, 40%), or large (>30 mm, 24%). The majority (88%) were basal cell carcinomas, with the lower eyelid most commonly affected (96%), particularly the medial canthus (50%). Reconstruction was successful in all 25 cases, with no evidence of tumour recurrence over a median follow-up period of 36 months. Reconstruction techniques included full-thickness skin grafts (upper inner arm: 64%; upper eyelid: 12%), upper eyelid tarsoconjunctival grafts with lower eyelid myocutaneous flaps (16%), the modified Hughes procedure (4%), and direct closure (4%). Complications requiring repeat surgical intervention occurred in 3 (12%) of cases, while minor complications managed conservatively occurred in 2 (8%). Post-operative issues included lagophthalmos (4%), medial ectropion (8%), and graft dehiscence (8%). Conclusion: Eyelid reconstruction post-Mohs surgery can be successfully performed through various techniques tailored to defect size, location, and lamella involvement. Asian eyelids with prominent medial epicanthal folds, may benefit from full-thickness skin grafts. Close coordination with the Mohs surgeon and timely defect closure are essential to optimizing results.
Keywords
Mohs Surgery, Eyelid Reconstruction.
Article Details
1. Introduction
Mohs micrographic surgery is a surgical technique used to excise skin cancers pioneered by Dr Frederic E. Mohs in the 1930s. In the late 1960s, Dr Mohs, along with Dr Theodore Tromovitch, introduced the fresh-frozen tissue technique used today [1]. It involves the excision of skin cancer with detailed evaluation of peripheral and deep margins in a single procedure. This technique allows precise mapping and orientation of the excised tissue, enabling targeted re-excision of microscopic tumour extensions while preserving healthy tissue [2].
By minimizing the removal of uninvolved tissue, Mohs surgery achieves high cure rates and optimal tissue conservation, making it the gold standard for removing basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) of the periocular region. However, Mohs surgery often results in complex defects that require careful reconstruction to restore both form and function to the eyelid [3].
Eyelid reconstruction after Mohs surgery presents unique challenges due to the delicate anatomy of the eyelid, which includes multiple lamellae and structures such as the tarsus, conjunctiva, and orbicularis muscle [4]. Depending on the size, depth, and location of the defect, a variety of reconstructive techniques may be employed, ranging from direct closure to more complex procedures such as full-thickness skin grafts or tarsoconjunctival flaps [5-7].
Asian eyelid anatomy presents unique challenges to reconstruction. Prominent medial epicanthal folds in Asian patients can obscure the medial canthus and complicate both defect visualization and graft placement. Asian patients also tend to have thicker skin and subcutaneous tissue in the lower eyelids, which can influence graft integration and flap mobility. The absence or minimal presence of a pre-tarsal crease in some individuals can complicate the aesthetic integration of grafts or flaps. Additionally, the more prominent orbital rim characteristic of Asian eyelids can influence contouring and alignment during reconstruction. Furthermore, the relatively tighter structure of the lower eyelid poses challenges in achieving proper closure and tension adjustments, particularly for larger defects. Finally, pigment variability between donor graft sites, such as the upper arm or inner eyelid, and the surrounding eyelid skin can result in noticeable colour mismatches, further complicating aesthetic outcomes [8-9].
In this study, we review a single institute's experience with eyelid reconstruction following Mohs surgery, focusing on patient outcomes, complication rates, and a comparison of the reconstructive techniques used. We also explore the impact of lesion size and location on the choice of technique and outcomes, as well as the potential influence of ethnicity on reconstructive choices in an Asian patient population.
2. Methods
2.1 Study Design
This was a retrospective study conducted at a single institution. The medical records of patients who underwent Mohs micrographic surgery (MMS) followed by eyelid reconstruction between January 1, 2014, and December 31, 2022, were reviewed. Institutional review board approval was obtained, and the study adhered to the tenets of the Declaration of Helsinki.
2.2 Patient Selection
Inclusion criteria were patients who underwent MMS for periocular skin cancers with subsequent eyelid reconstruction. Patients with prior eyelid surgeries or underlying ocular pathologies that could affect outcomes were excluded. A total of 25 patients met the inclusion criteria.
2.3 Data Collection
Demographic data, including age, sex, and ethnicity, were recorded. Lesion characteristics, including size (small: <20 mm, medium: 20–30 mm, large: >30 mm), location (upper, lower, medial canthus, lateral canthus), and histological type (basal cell carcinoma, squamous cell carcinoma, sebaceous carcinoma), were documented. Surgical techniques employed for reconstruction were categorized, including full-thickness skin grafts, tarsoconjunctival flaps, the Hughes procedure, and direct closure. Post-operative complications, including lagophthalmos, ectropion, and graft failure, were recorded, as well as recurrence rates.
2.4 Statistical Analysis
Descriptive statistics were used to summarize demographic and clinical data. Fisher's exact test was employed to assess the relationship between lesion size, location, surgical technique, and complication rates. Statistical significance was defined as p < 0.05.
3. Results
3.1 Patient Demographics
The mean patient age was 67.2 years, ranging from 49 to 89 years. Of the 25 patients, 18 (72%) were male and 7 (28%) were female. The majority (68%) were of Chinese ethnicity, with the remaining (32%) representing other racial groups. 2 of the patients had a significant background of schizophrenia and one had a significant history of recurrent basal cell carcinomas (having more than 250 basal cell carcinomas since the age of 25, with previous genetic testing inconclusive for Gorlin syndrome).
3.2 Lesion Characteristics
The majority of lesions were basal cell carcinomas (88%), with smaller numbers of squamous cell carcinomas (4%) and sebaceous gland carcinomas (8%). Most lesions (96%) were located on the lower eyelid, and 50% involved the medial canthus. Lesions were classified as small (<20 mm, 36%), medium (20–30 mm, 40%), or large (>30 mm, 24%). 2 (8%) of the cases were recurrent.
3.3 Surgical Techniques
The most common reconstructive technique was full-thickness skin grafts, which were used in 64% of cases, typically harvested from the upper inner arm or upper eyelid. Tarsoconjunctival grafts combined with lower lid myocutaneous flaps were used in 16% of patients. Other techniques included the modified Hughes procedure (4%) and direct closure (4%). Majority of cases were closed 1 day after excision (92%), 1 case was closed on the same day (4%) and 1 case was closed 2 days after excision (4%).
3.4 Outcomes and Complications
Reconstruction was successful in all 25 cases, with no evidence of tumour recurrence over a median follow-up period of 36 months. Complications occurred in 5 patients (20%): 1 patient experienced post-operative lagophthalmos, 2 developed medial ectropion, and 2 had graft dehiscence. The 2 cases of dehiscence were repaired surgically. One case with medial ectropion and lagophthalmos was managed surgically with a repeat anterior lamellar graft. 2 cases of medial ectropion were mild and were managed conservatively. There was no statistically significant association between complication rates and lesion size, location, or the reconstructive technique employed (p > 0.05).
3.5 Patients with medial canthus lesions
A total of 7 patients had medial canthus defects, of which 5 were Chinese and 2 were Caucasian. 7 underwent reconstruction with full thickness skin graft from the upper inner arm, and 1 from the upper eyelid. 1 Caucasian patient developed medial ectropion post-operatively. Photographs of his case would be detailed in the section regarding complications.
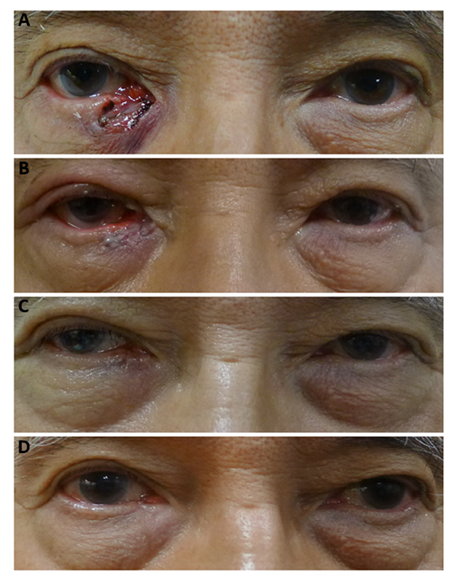
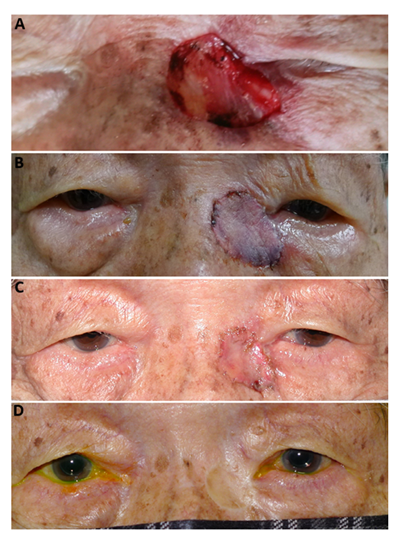
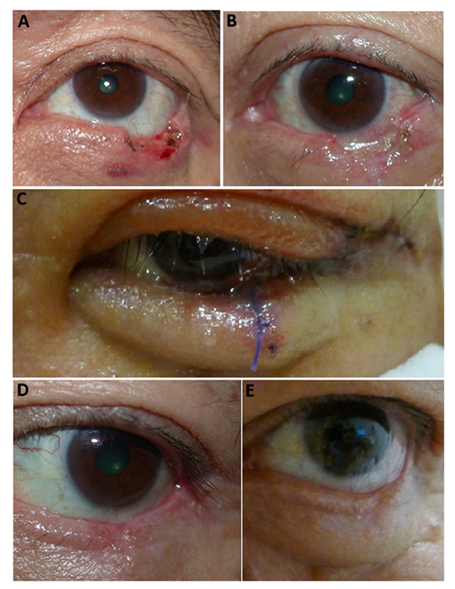
The first patient with a medial canthus defect was a 70-year-old gentleman with a 12x10mm defect post Mohs for basal cell carcinoma. The defect was closed with a full thickness skin graft from the patient’s right upper eyelid. Pre- and post-operative photographs show good wound healing with no complications. (Figure 1).
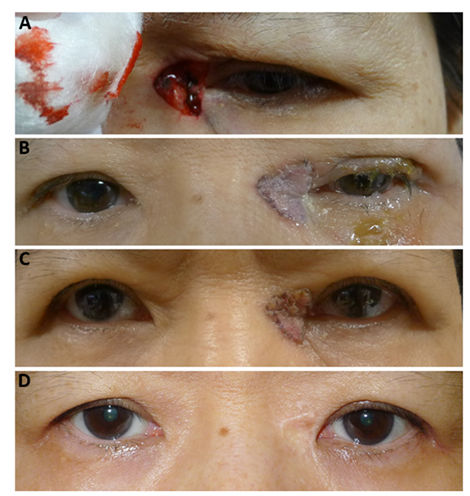
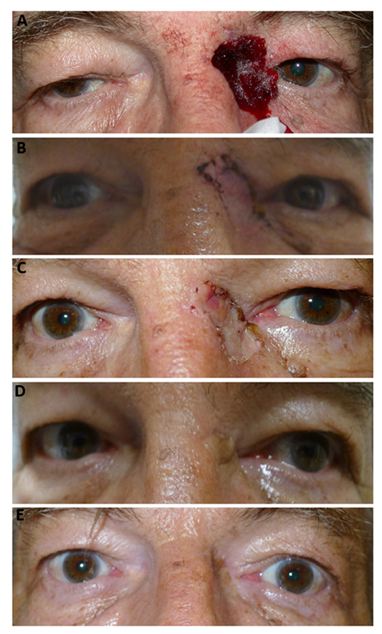
The second patient was a 60-year-old Chinese female with a 12x10mm medial canthus defect post excision for basal cell carcinoma. The defect was closed with a full thickness skin graft from the patient’s left upper inner arm. Pre- and post-operative photographs show good wound healing with no complications. The epicanthal fold was preserved. (Figure 2).
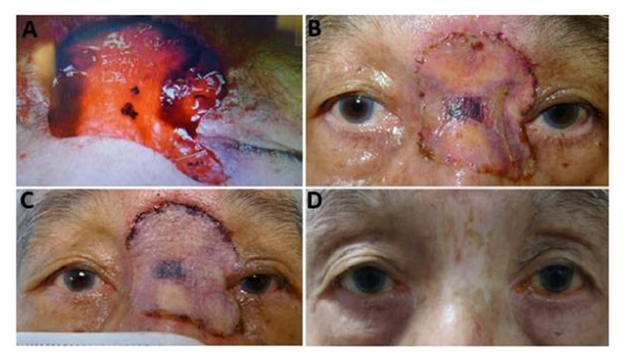
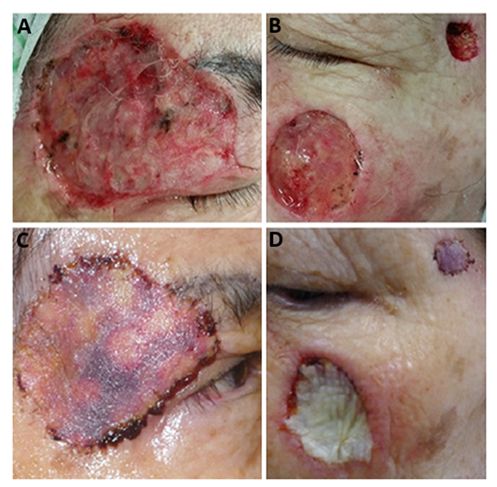
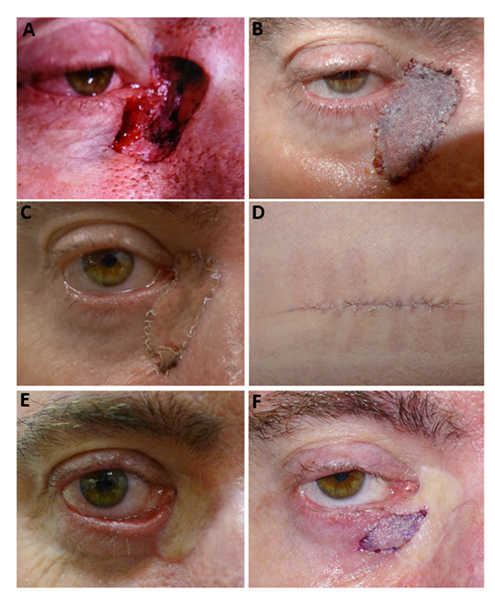
The third patient was a 78-year-old gentleman with a large 48x42mm defect over the nose involving both medial canthus more on the left than the right. The defect was closed with a full thickness skin graft from the patient’s left upper inner arm. Pre- and post-operative photographs show good wound healing with slight hypopigmentation of the skin remaining. (Figure 3)
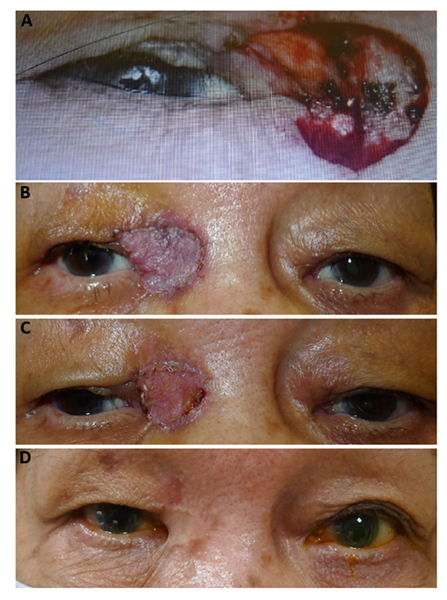
The fourth patient was a 77-year-old Chinese lady with a deep 20x18mm medial canthal defect post excision for basal cell carcinoma. The defect was closed with a full thickness skin graft from the patient’s left upper inner arm. Pre- and post-operative photographs show good wound healing with slight hypopigmentation of the skin remaining. (Figure 4)
The fifth patient was an 83-year-old chinses gentleman who had a 23mmx16mm left medial canthus defect post excision for basal cell carcinoma. The defect was closed with a full thickness skin graft from the patient’s left upper inner arm. Pre- and post-operative photographs show good wound healing with slight hypopigmentation of the skin remaining. (Figure 5)
The sixth patient was a 61-year-old Caucasian gentleman with a 50x40mm medial canthus defect post excision for basal cell carcinoma. The defect was closed with a full thickness skin graft from the patient’s left upper inner arm. Pre and post-operative photographs show good wound healing with no complications (Figure 6).
3.6 Cases with complications
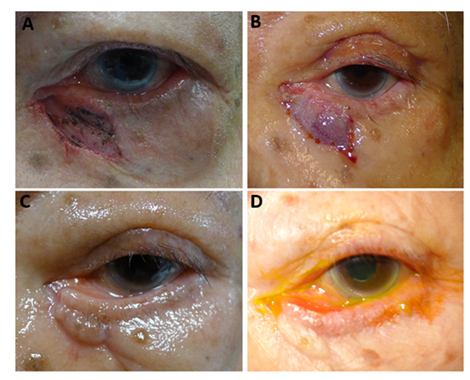
The first case of graft dehiscence was a 71-year-old female patient with squamous cell carcinoma over multiple sites. She was left with defects over her right upper eyelid and temple measuring 51x45mm, left cheek measuring 26x26mm and left temple measuring 12x11mm. The defects were closed using full thickness skin grafts from her left upper arm. (Figure 7A) The left cheek graft was noted to be slightly dehisced & stretched after inadvertent rubbing 13 days post operatively. She underwent repeat re-suturing and had adequate graft healing thereafter. (Figure 7b).
Figure 7a: A: Pre-operative image of defect over her right upper eyelid and temple measuring 51x45mm B: Pre-operative image of defects over her left cheek measuring 26x26mm and left temple measuring 12x11mm C and D: Post-operative image of defects repaired with full thickness skin graft from upper inner arm.
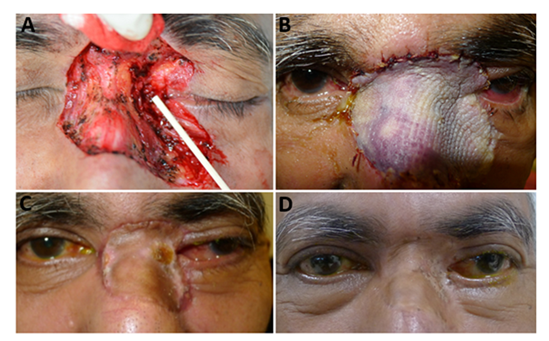
The second case of dehiscence was a 65-year-old Chinese male with a left lower eyelid basal cell carcinoma. He had a small 10mm x 6mm lateral lower lid defect post MOHs surgery that was closed via direct closure. There was noted to be dehiscence of sutures at post-op day 5 and the patient underwent repeat closure of the left lower lid defect with a Tenzel semicircular flap (Figure 8).
B: Post-operative day 5 photo showing dehiscence of sutures C: Post-operative photo after repeat closure of the left lower lid defect with a Tenzel semicircular flap D: Post-operative photo 1 month later E: Post-operative photo 6 months later.
The case with post-operative ectropion with lagophthalmos was a 47-year-old Caucasian gentleman with history of recurrent basal cell carcinomas. He had a right 25x15mm medial canthus defect post excision of BCC. The defect was repaired with a full thickness skin graft from the left upper arm. Post operatively there was medial lower lid ectropion with lagophthalmos which was repaired with full thickness skin graft. The patient was lost to follow-up after the second surgery. (Figure 9)
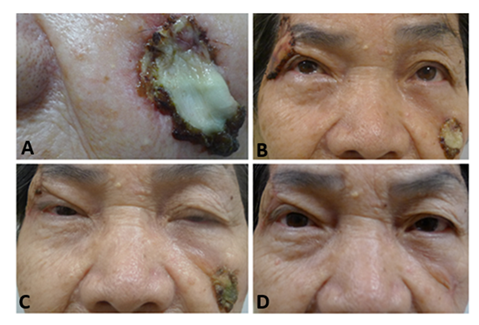
The first case of medial ectropion was a 86-year-old Chinese gentleman with history of schizophrenia who had a 20mm x 10mm left medial lower eyelid defect post basal cell carcinoma excision. The defect was repaired with full thickness skin graft from his left upper eyelid. He had a lower eyelid medial ectropion from graft contracture which was conservatively managed (Figure 10).
The second case of medial ectropion was a 54-year-old Indian gentleman with history of schizophrenia who underwent excision of basal cell carcinoma over his nose. He had a resulting large 60x50 mm defect over nose & medial canthus, with residual tumour remaining over left medial canthus. He underwent a left medial canthus tumour excision biopsy and medial canthus and nasal bridge reconstruction with full thickness skin graft. Post operatively he developed a mild medial ectropion of his left lower eyelid which was conservatively managed (Figure 11).
4. Discussion
Eyelid reconstruction following Mohs surgery in Asian patients requires careful consideration of both the functional and aesthetic aspects of the eyelid [10]. The upper eyelid crease is formed by the fascial extensions of the levator aponeurosis, which pass through the orbicularis oculi muscle to attach to the skin. The aponeurosis also attaches inferiorly to the anterior tarsal plate, with the crease running parallel to the eyelid margin. Typically, the upper eyelid crease is located 8–9 mm above the margin in men and 8–11 mm in women. In Asian eyelids, the crease is less defined, positioned 2–3 mm above the margin due to the absence of fascial extensions and a lower aponeurotic insertion on the tarsal plate. The lower eyelid crease is subtler, starting medially 4–5 mm below the margin and extending inferolaterally. It forms via fascial extensions of the capsulopalpebral fascia, which are absent in the lower eyelids of Asians, resulting in the absence of a defined crease [9,11].
The epicanthal fold, a crescent-shaped skin fold at the medial aspect of the upper eyelid, extends along the nose toward the medial canthus and connects with the lower eyelid. This structure is present in nearly all newborns but persists into adulthood in 90% of Asians and only 2% of non-Asians. It also contributes to a wider intercanthal distance [12].
In 1968, Johnson introduced a classification system for epicanthal folds, categorizing them into four distinct subtypes [13]:
1. Type I: Epicanthus Supraciliaris
- • Originates at the brow and curves concavely toward the lacrimal sac.
- • The lacrimal sac and caruncle remain exposed.
2. Type II: Epicanthus Palpebralis
- • Arises from the upper eyelid and extends downward.
3. Type III: Epicanthus Tarsalis
- • Initiates at the upper eyelid crease and converges with the medial canthus.
- • This is the most prevalent subtype in Asians and often conceals the lacrimal lake and caruncle.
4. Type IV: Epicanthus Inversus
- • Originates from the lower eyelid and extends medially and upward, distinguishing it from the other subtypes.
Our study looks into the role of ethnicity in reconstructive choices. Asian patients with more prominent epicanthal folds may benefit from using full-thickness skin grafts. Prominent epicanthal folds can make reconstruction challenging, especially when the intercanthal distance needs to be preserved or corrected. Full-thickness grafts can provide good pliability and shape retention to accommodate this and are less prone to contraction compared to split-thickness grafts [14]. The initial differences in the texture and colour of the eyelid skin compared to the inner arm skin tend to fade over time and provide an acceptable cosmetic outcome [15].
Complications requiring repeat surgery in this study was 12% while rate of minor complications managed conservatively was 8%. 2 cases of medial ectropion were considered minor and were managed conservatively, but 1 case with lagophthalmos and ectropion and the 2 cases of graft dehiscence required repeat surgery for adequate closure. These complications rates and findings are consistent with other reports, which suggest that complications are more likely in larger or medial defects due to the anatomical complexity of the region [16-18]. However, we did not observe a significant relationship between lesion size, location, or technique and complication rates, suggesting that proper technique selection can mitigate these risks.
In a study looking at free tarsoconjunctival graft (FTG) transplantation for East Asian eyelids by Ominato et al in 2022, 42 cases reconstructed with FTG, the upper eyelid was reconstructed in 23. Postoperative complications were observed in 12 cases (52%): entropion in eight and corneal epithelial disorder in four. Revision surgery was required in three of those cases (13%). There were 19 cases of lower eyelid reconstruction. Postoperative complications were observed in seven cases (32%): ectropion in three and corneal epithelial disorder in two and one lower eyelid ptosis. Two of these cases (11%) required revision surgery [16].
Zlatarova et al evaluated 39 patients who underwent lid reconstruction with full thickness skin grafts and found that 95% of the cases the skin grafts were viable, of which graft failure occurred two patients because of subcutaneous haematoma. Other early postoperative complications including graft contraction (3 patient), graft hypertrophy (5 patients), and partial graft failure (3 patients) were managed without surgery [17].
In systemic review done by Archibald et al, reconstructive methods were reported for 3678 cases and included linear repair (18%), advancement flap (8%), rotation flap (5%), transposition flap (3%), island pedicle flap (1%), unspecified local skin flap (21%), skin graft (23%), secondary intention (4%), tarsoconjunctival flap (3%), and combined reconstruction techniques (13%), showing local skin flaps and grafts were the most utilized techniques [18].
With regards to complications post reconstruction, Balchev reported on a cohort of 450 tumours operated that revealed 13 (2.8%) operations with recurrences and 32 (7%) with complications. Complications included: ectropion, dehiscence, gross cicatrix with normal function, retraction, post-radiation damage, sub-graft haemorrhage and graft rejection [19]. These findings were consistent with what we observed in our cohort. Rates of recurrences following surgery were also consistent with previously published data, supporting the high success rate of Mohs surgery [20-22].
Coordination between the Mohs surgeon and the reconstructive surgeon is crucial, particularly in cases requiring immediate reconstruction. Early closure of defects minimizes the risk of wound contracture and scar formation, leading to better functional and aesthetic outcomes.
5. Conclusion
Eyelid reconstruction following Mohs micrographic surgery is associated with high success rates and low recurrence when appropriate techniques are employed based on the defect's size, location, and lamellar involvement. Full-thickness skin grafts, particularly in Asian populations, offer favourable outcomes for defects involving the medial canthus. Close coordination between the surgical teams and early defect closure are key to optimizing patient outcomes.
Declaration of Interest Statement:
The authors report no conflict of interest.
Funding:
There were no sources of funding or financial support for this project.References
- Mansouri B, Bicknell LM, Hill D, et al. Mohs Micrographic Surgery for the Management of Cutaneous Malignancies. Facial Plast Surg Clin North Am 25 (2017): 291-301.
- Vuyk H D, Lohuis P J. Mohs micrographic surgery for facial skin cancer. Clin Otolaryngol Allied Sci 26 (2001): 265–273.
- Huggins AB, Latting MW, Marx DP, et al. Ocular Adnexal Reconstruction for Cutaneous Periocular Malignancies. Semin Plast Surg 31 (2017): 22-30.
- Yan Y, Fu R, Ji Q, et al. Surgical Strategies for Eyelid Defect Reconstruction: A Review on Principles and Techniques. Ophthalmol Ther 11 (2022): 1383-1408.
- Yamamoto N, Ogi H, Yanagibayashi S, et al. Eyelid reconstruction using oral mucosa and ear cartilage strips as sandwich grafting. Plast Reconstr Surg Glob Open 5 (2017): e1301.
- Holds JB. Lower eyelid reconstruction. Facial Plast Surg Clin Nam 24 (2016): 183–191.
- Trieu DN, Drosou A, White LE, et al. Outcomes of Second Intention Healing of the Lower Eyelid Margin After Mohs Micrographic Surgery. Dermatol Surg 45 (2019): 884-889.
- Jeong S, Lemke BN, Dortzbach RK, et al. The Asian upper eyelid: an anatomical study with comparison to the Caucasian eyelid. Arch Ophthalmol 117 (1999): 907-912.
- Saonanon P. Update on Asian eyelid anatomy and clinical relevance. Curr Opin Ophthalmol 25 (2014): 436-442.
- Ahmad J, Mathes DW, Itani KM. Reconstruction of the eyelids after mohs surgery. Semin Plast Surg 22 (2008): 306-318.
- Sun M, Andrea J, John P, et al. Tissue Engineering in Ophthalmology: Implications for Eyelid Reconstruction. Ophthalmic Plastic and Reconstructive Surgery 33 (2017): 157-162.
- Wu XS, Jian XC, He ZJ, et al. Investigation of anthropometric measurements of anatomic structures of orbital soft tissue in 102 young han chinese adults. Ophthalmic Plast Reconstr Surg 26 (2010): 339-43.
- Johnson CC. Epicanthus. Am J Ophthalmol 66 (1968): 939-946.
- Adams DC, Ramsey ML. Grafts in dermatologic surgery: review and update on full- and split-thickness skin grafts, free cartilage grafts, and composite grafts. Dermatol Surg. 2005 Aug;31(8 Pt 2):1055-67.
- Rigg BM. Importance of donor site selection in skin grafting. Can Med Assoc J 117 (1977): 1028-1029.
- Ominato J, Oyama T, Cho H, et al. Evaluation of the postoperative course of East Asian eyelid reconstruction with free tarsoconjunctival graft transplantation: A Japanese single-centre retrospective study. JPRAS Open 33 (2022): 6-16.
- Zlatarova ZI, Nenkova BN, Softova EB. Eyelid Reconstruction with Full Thickness Skin Grafts After Carcinoma Excision. Folia Med (Plovdiv) 58 (2016): 42-47.
- Archibald LK, Gupta R, Shahwan KT, et al. Periorbital reconstructive techniques following Mohs micrographic surgery or excisions: a systematic review. Arch Dermatol Res 315 (2023): 1853-1861.
- Balchev G. Complications and Recurrences after Excision and Reconstruction of Eyelid Tumours. Curr Oncol 31 (2024): 1713-1724..
- Hartley MJ, Meredith PR, Oliphant T. Outcomes of Mohs micrographic surgery for periocular squamous cell carcinoma. Eur J Ophthalmol 34 (2024): 1506-1510.
- Golda N, Hruza G. Mohs Micrographic Surgery. Dermatol Clin 41 (2023): 39-47.
- Weesie F, Naus NC, Vasilic D, et al. Recurrence of periocular basal cell carcinoma and squamous cell carcinoma after Mohs micrographic surgery: a retrospective cohort study. Br J Dermatol 180 (2019): 1176-1182.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
