High Frequency Variability Index as an Early Indicator of Fluid Resuscitation During Gynecologic Surgery: A Case Report
Mitsutaka Edanaga M.D, Ph. D1*, Motonobu Kimizuka M.D, Ph. D1, Mako Doumi D.D.S2, Akihiro Miyazaki D.D.S, Ph. D2, Michiaki Yamakage M.D, Ph. D1
1Department of Anesthesiology, Sapporo Medical University School of Medicine, Sapporo, Hokkaido, Japan
2Department of Oral Surgery, Sapporo Medical University School of Medicine, Sapporo, Hokkaido, Japan
*Corresponding Author: Mitsutaka Edanaga, Department of Anesthesiology, Sapporo Medical University School of Medicine, Sapporo, Hokkaido, Japan.
Received: 18 June 2025; Accepted: 23 June 2025; Published: 13 August 2025
Article Information
Citation: Mitsutaka Edanaga, Motonobu Kimizuka, Mako Doumi, Akihiro Miyazaki, Michiaki Yamakage. High Frequency Variability Index as an Early Indicator of Fluid Resuscitation During Gynecologic Surgery: A Case Report. Anesthesia and Critical care 7 (2025): 49-52.
View / Download Pdf Share at FacebookAbstract
Background: High Frequency Variability Index (HFVI), derived from heart rate variability (HRV), is an indicator of parasympathetic nervous activity. Recently, HFVI has been used as an objective marker of analgesia, with values above 50 generally indicating adequate pain relief. In this report, we present the first case in which HFVI served as a prompt indicator for initiating fluid resuscitation during intraoperative hemorrhage.
Case: A woman in her 40s was scheduled to undergo a radical abdominal hysterectomy. In addition to standard vital signs monitoring, HFVI was used to adjust the dosage of remifentanil. Following epidural catheterization, general anesthesia was induced. Anesthesia was maintained with 1.3 L/min of Air, 0.7 L/min of O2 and 1.5% of sevoflurane (end-tidal concentration: 1.0%). Only the remifentanil dosage was modified based on HFVI readings. Approximately 150 minutes after the start of surgery, the systolic blood pressure frequently dropped below 80 mmHg, and phenylephrine was administrated several times. HFVI values fell below 50, followed by a gradual increase in heart rate. In response to suspected hypovolemia, fluid resuscitation was performed using crystalloid solution and Voluven®. After treatment, HFVI values rose above 50 and remained stable. Notably, vital sign may not change until significant blood loss has occurred, whereas parasympathetic withdrawal may appear earlier in the course of hemorrhage.
Conclusion: HFVI may serve as a useful early indicator for initiating fluid resuscitation during intraoperative hemorrhage.
Keywords
<p>High frequency variability index; Parasympathetic nervous activity; Intraoperative hemorrhage; Fluid resuscitation</p>
Article Details
Abbreviation: HFVI: High Frequency Variability Index; HRV: heart rate variability; HFVIi: Component i of High Frequency Variability Index; HFVIm: Component m of High Frequency Variability Index; PAC: pulmonary artery catheter; TEE: transesophageal echocardiography
1. Introduction
Changes in vital sign during intraoperative hemorrhage are typically characterized by a decrease in blood pressure and increase in heart rate. However, these hemodynamic changes tend to occur only after a significant amount of blood loss has accumulated. In other word, blood pressure and pulse rate can generally be maintained until approximately 15 % of total blood volume is lost [1,2]. Therefore, it is crucial to detect changes in circulating blood volume at an early stage and alert the anesthesiologist accordingly. While invasive arterial pressure monitoring is commonly used in patients with unstable hemodynamics [3], devices such as Flotrac™/Vigileo™ [4] and LiDCO™ [5] have been considered useful tools for minimally invasive cardiac output monitoring, as they allow for real time analysis of arterial pressure waveforms. However, such monitoring is typically reserved for high-risk patients [6], generally those classified as ASA-PS III [7].
The High Frequency Variability Index (HFVI) has been introduced as a component of the analgesia-nociception index [8]. HFVI is derived from heart rate variability (HRV) and reflects the high-frequency component associated with parasympathetic nervous activity [9]. Previous studies have suggested that HFVI can serve as an objective indicator of both pain and pain relief [10]. In this report, we present a case in which HFVI acted as a prompt indicator for initiating fluid resuscitation therapy during gynecologic surgery complicated by intraoperative hemorrhage.
2. Case Report
Written informed consent was obtained from the patients for publication of this case. A-46-year-old woman was admitted to the gynecological ward of Sapporo Medical University Hospital for the management of cervical cancer. She was scheduled to undergo a radical abdominal hysterectomy. Her preoperative hemoglobin level was 12.2 g/dL, indicating no anemia. She was classified as American Society of Anesthesiologist Physical Status I, and epidural catheterization and general anesthesia were planned. Additionally, HFVI monitoring was incorporated to assist in adjusting remifentanil dosage. Upon arrival in the operating room, the HFVI MOC-9 module® (Heiwa Bussan, Tokyo, Japan) and HFVI V1 plus sensor® were attached to the precordial region and connected to a Root monitor (Mashimo Co., Tokyo, Japan). HFVI consists of two components: HFVIi, the average over 1-2 minutes, and HFVIm, the average over 2-4 minutes. HFVIi is regarded as a sensitive indicator of rapid changes in heart rate variability, while HFVIm is more stable and useful for titrating analgesics. After epidural catheterization at the T 12/L 1 interspace, general anesthesia was induced with 2 mg/kg propofol and 0.7 mg/kg rocronium. Sevoflurane at 3% was administrated for 2 minutes prior to intubation. Following tracheal intubation with a standard laryngoscope, anesthesia was maintained with 1.3 L/min air, 0.7 L/min oxygen, and 1.5% sevoflurane (end-tidal concentration: 1.0%). No epidural anesthetics were administrated until the end of surgery; intraoperative analgesia was managed solely by adjusting based on HFVI reading. A radial arterial line was placed, and vital sign were recorded every 5 minutes. HFVIm and HFVIi were continuously displayed on the Root monitor.
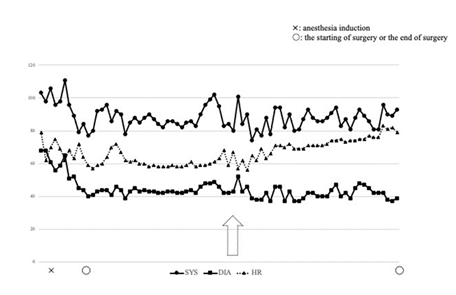
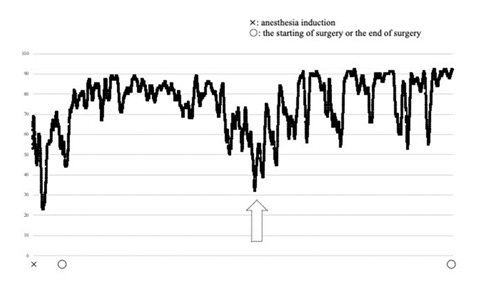
Approximately 150 minutes after the start of surgery, systolic blood pressure frequently fell below 80 mmHg (Figure 1), prompting repeated administration of phenylephrine. At the same time, HFVI values dropped below 50, and heart rate gradually increased from the 50s to 60s. Blood loss gradually increased from 200 to 540 mL. Fluid resuscitation therapy was initiated using crystalloid solution and Voluven® (Otsuka Pharmaceutical Factory, Inc., Naruto, Tokushima, Japan) of hydroxyethyl starch. On two separate occasions, HFVIm dropped below 50 (Figure 2), reinforcing the suspicion of ongoing hypovolemia. Although the total blood loss had reached 690 mL by one hour after active hemorrhage began, HFVIm rose above 50 and remained stable thereafter. Total intraoperative blood loss was 900 mL, and urine output was 200 mL. The patients received 2200 mL of crystalloid solution (including 200 mL of normal saline) and 500 mL of Voluven. At the end of the procedure, her blood pressure was 93/39 mmHg and heart rate was 79 bpm. The patient regained consciousness promptly and was extubated without complications.
Figure 1: Changes in blood pressure and heart rate in the perioperative period. Heart rate gradually increased following intraoperative hemorrhage. Systolic blood pressure: circle markers (solid line). Diastolic blood pressure: square markers (solid line). Heart rate: triangle markers (dotted line).
Figure 2: Changes in HFVIm in the perioperative period. Component m of High Frequency Variability Index (HFVI) represents the average value over 2-4 minutes. HFVIm decreased below 50 during intraoperative hemorrhage (indicated by an upward dotted arrow). Cross marker indicates the time of anesthesia induction. Circle marker indicates the start or the end of surgery.
3. Discussion
During intraoperative hemorrhage, blood pressure and heart rate may remain stable in the early phase until more than 15 % of the circulation blood volume is lost. In the other words, traditional vital signs may fail to promptly reflect hemodynamic instability. We cannot immediately realize hemodynamic instability at intraoperative hemorrhage. Therefore, early detection of reduced circulating volume is essential to initiate timely intervention. A previous systemic review on optimal anesthetic monitoring after liver transplantation [11] recommended the use of pulmonary artery catheter (PAC) and/or transesophageal echocardiography (TEE) for high-risk patients. In contrast, minimally invasive cardiac output monitors such as Flotrac™/Vigileo™ and LiDCO™ have not been shown to offer comparable reliability in unstable cases. Nonetheless, the other report [12] suggests that goal-directed fluid therapy using such monitors in noncardiac surgery may reduce hospital stay. However, it remains unclear whether these minimally invasive cardiac output monitoring are sensitive enough to detect early phase of intraoperative hemorrhage [13].
To our knowledge, no previous case reports have described HFVI as an early indicator for fluid therapy. HFVI has been used to objectively assess nociception, based on the physiological relationship where pain activates the sympathetic nervous system [14] and analgesia promotes parasympathetic activity. HFVI has been used for pain relief during various operations. [15,16] Autonomic regulation of the cardiovascular system plays a compensatory role in hemorrhage states. [17] In early hemorrhage, parasympathetic withdrawal and sympathetic activation lead to increase heart rate and peripheral resistance, maintaining blood pressure despite ongoing volume loss. The previous study [18] found that HRV has been recognized as a marker of autonomic compensation in trauma patients.
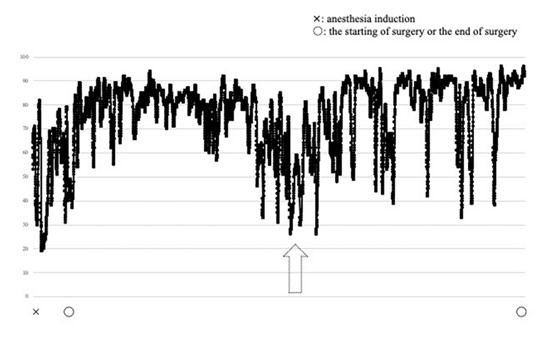
In our case, despite intraoperative hemorrhage, HFVIi showed an early decline (Figure 3), followed by HFVIm. These findings suggest that HFVIm may serve as a prompt, noninvasive indicator for initiating fluid resuscitation during intraoperative hemorrhage. A prospective study is warranted to validate these findings [19,20].
Figure 3: Changes in HFVIi in the perioperative period. in the perioperative period. Component i of High Frequency Variability Index (HFVIi) represents the average value over 1-2 minutes. HFVIi decreased below 50 ahead of HFVIm. Cross marker indicates the time of anesthesia induction. Circle marker indicates the start or the end of surgery. Upward dotted arrow was the time in which HFVIm decreased below 50.
4. Conclusion
We reported a case of anesthesia management using HFVI monitoring for intraoperative hemorrhage during gynecologic surgery. Considering the rapid changes in heart rate variability observed during blood loss, HFVIm may serve as a prompt indicator for initiating fluid resuscitation [21-25]. Although HFVI is primarily used to adjust analgesic dosing it may also be useful in identifying early hemodynamic instability.
Acknowledgements
The acquired data of High Frequency Variability Index was supported by Yasufumi Majima and Takashi Yamauchi, Heiwa Bussan Co., Tokyo, Japan.
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Mutschler M, Paffrath T, Wolfl C, et al. The ATLS classification of hypovolemic shock: A well established teaching tool on the edge. Injury 45 (2014): S35-S38.
- Pacagnella RC, Souza JP, Durocher J, et al. A systematic review of the relationship between blood loss and clinical signs. PLoS ONE 8 (2013): e57594.
- Daisuke H, Ryota S, Abhijit D, et al. Comparison of central and peripheral arterial blood pressure gradients in critically ill patients: a systematic review and meta-analysis. Crit Care Explor 6 (2024): e1096.
- Compton FD, Zukunft B, Hoffmann C, et al. Performance of a minimally invasive uncalibrated cardiac output monitoring system (FlotracTM/VigileoTM) in haemodynamically unstable patients. Br J Anaesth 100 (2008): 451-6.
- Moharari RS, Shahinpour S, Etezadi F, et al. Comparison of goal-directed fluid therapy using LiDCO rapid system with regular fluid therapy in patients undergoing spine surgery as a randomized clinical trial. RJAIC 112 (2014): 648-659.
- Reza SM, Shervin S, Farhad E, et al. LiDCO system with regular fluid therapy in patients undergoing spine surgery as a randomized clinical trial. Rom J Anaesth Intensive Care 28 (2022): 1-9.
- Arulkumaran N, Corredor C, Hamilton MA, et al. Cardiac complications associated with goal-directed therapy in high-risk surgical patients: a meta-analysis. Br J Anaesth 112 (2014): 648-659.
- Pearse RM, Moreno RP, Bauer P, et al. Mortality after surgery in Europe: a 7 day cohort study. Lancet 380 (2012): 1059-1065.
- Boseli E, Bouvet L, Be´gou G, et al. Prediction of immediate postoperative pain using the analgesia/nociception index: a prospective observational study. Br J Anaesth 112 (2014): 715-721.
- Keisuke Y, Shinju O, Satoki I. Analgesia nociception index and high frequency variability index: promising indicators of relative parasympathetic tone. J Anesth 37 (2023): 130-137.
- Bill H, Yusef S, Alexa C, et al. Objective monitoring of pain using high frequency heart rate variability-a narrative review. Digital Medicine and Healthcare Technology 3 (2024): 1-17.
- Thomas MAF, Nick S, Claus GK, et al. What is the optimal anesthetic monitoring regarding immediate and short-term outcomes after liver transplantation?- a systematic review of the literature and expert panel recommendations. Clinical Transplantation 36 (2022): e14643.
- Marie KJ, Mikael FV, Mathias JH, et al. Goal-directed haemodynamic therapy during general anaesthesia for noncardiac surgery: a systematic review and meta-analysis. Br J Anaesth 128 (2022): 416-433.
- Lee AJ, Cohn JH, Ranasinghe JS. Cardiac output assessed by invasive and minimally invasive techniques. Anesthesiol Res Pract 2021 (2011): 475151.
- Hannibal KE, Bishop MD. Chronic stress, cortisol dysfunction, and pain: a psychoneuroendocrine rationale for stress management in pain rehabilitation. Phys Ther 94 (2014): 1816-1825.
- Jeanne M, Cle ´ment C, De Jonckheere J, et al. Variations of the analgesia nociception index during general anaesthesia for laparoscopic abdominal surgery. J Clin Monit Comput 26 (2012): 289-294.
- Motoki K, Naoto Y, Masahiro W, et al. Effect of postoperative peripheral nerve blocks on the analgesia nociception index under propofol anesthesia: an observational study. J Clin Monit Comput Online ahead of print (2025).
- Li C, Chiluwal A, Afridi A, et al. Trigeminal nerve stimulation: a novel method of resuscitation for hemorrhage shock. Crit Care Med 47 (2019): e478-e84.
- William HC, Jose S, Victor AC, et al. Heart rate variability and its association with mortality in prehospital trauma patients. J Trauma 60 (2006): 363-370.
- Adrienne LA, Christian EW, Eric LG, et al. The role of heart rate variability in mindfulness-based pain relief. The Journal of Pain 21 (2020): 306-323.
- Boseli E, Bouvet L, Be´gou G, et al. Prediction of immediate postoperative pain using the analgesia/nociception index: a prospective observational study. Br J Anaesth 112 (2014): 715-721.
- Boseli E, Daniela-Ionescu M, Be´gou G, et al. Prospective observational study of the non-invasive assessment of immediate postoperative pain using the analgesia/nociception index. Br J Anaesth 111 (2013): 453-459.
- Nelson A, Raquel MR. Pain and the autonomic nervous system. The role of non-invasive neuromodulation with NEA microcurrents. Front Pain Res 6 (2025): 1410808.
- Henry DU, Guy LL, Andrew W, et al. Intraoperative “analgesia nociception index”-guided fentanyl administration during sevoflurane anesthesia in lumbar discectomy and laminectomy: a randomized clinical trial. Anesth Analg 125 (2017): 81-90.
- https://www.jkri.or.jp/PDF/2016/sogo_73_kagawa.pdf
Related PubMed Articles
- Perioperative liberal drinking management promotes postoperative gastrointestinal function recovery after gynecological laparoscopic surgery: A randomized controlled trial.
- Reversible Acute Kidney Injury Due to Suspected Paraneoplastic Glomerulopathy in Malignant Ovarian Germ Cell Tumor: A Case Report.
- Fluid resuscitation dilemma: anticipating massive blood loss in hysterectomy.
- Amniotic fluid embolism in late second trimester abortion: a case report.
- Perioperative liberal drinking management promotes postoperative gastrointestinal function recovery after gynecological laparoscopic surgery: A randomized controlled trial.
- Effects of intraoperative esketamine addition on gastrointestinal function after benign gynaecological laparoscopic surgery: a double-blind, randomized controlled study.
- Critical Care in Placenta Accreta Spectrum Disorders-A Call to Action.
- Corrected flow time and respirophasic variation in blood flow peak velocity of radial artery predict fluid responsiveness in gynecological surgical patients with mechanical ventilation.
- Successful treatment of cardiac arrest following hysteroscopic surgery using extracorporeal membrane oxygenation: A case report.
- Acute postoperative delayed hemorrhage following anterior colporrhaphy and cystoscopy: A case report and a review of the literature.
- Life-threatening acute water intoxication in a woman undergoing hysteroscopic myomectomy: a case report and review of the literature.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 77.58%
Acceptance Rate: 77.58%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 