Effectiveness of Negative Pressure Wound Therapy in Managing Post-Surgical Wounds
Itedal Albani*,1, Aateka Fatima Mohammed2, Zahraa Al Samsam3, Melak Al-Sammarraie4, Alyazey Hasan Alrammah3, Jamal Mohammed Kunhi5, Mohamed Mobark Obed Yousif6, Mehrun Nissa Shaikh4, Ayesha sajid7, Asra’a Alnakeb8, Muhammad Salman Arif9
1University of Sharjah, clinical teaching fellow
2Umm Al quwain hospital
3University of Sharjah
4Ajman university
5Tbilisi state medical university
6Bayan University
7 Khaja Bandanawaz institute of medical sciences
8Dubai Medical College for Girls
9Shifa international hospital
*Corresponding Author: Itedal Albani, University of Sharjah, clinical teaching fellow, UAE
Received: 30 April 2025; Accepted: 07 April 2022; Published: 13 May 2025
Article Information
Citation: Itedal Albani, Aateka Fatima Mohammed, Zahraa Al Samsam, Melak Al- Sammarraie, Alyazey Hasan Alrammah, Jamal Mohammed Kunhi, Mohamed Mobark Obed Yousif, Mehrun Nissa Shaikh, Angana raveendran prathapan, Asra’a Alnakeb, Muhammad Salman Arif. Effectiveness of Negative Pressure Wound Therapy in Managing Post-Surgical Wounds. Journal of Surgery and Research. 8 (2025): 260-264.
View / Download Pdf Share at FacebookAbstract
In the treatment of surgical and chronic wounds, Negative Pressure Wound Therapy (NPWT) has become a popular technique. There are various researches available which aim to study its efficacy and clinical outcome. However, different study designs and contrasting results call for a thorough and comprehensive study which analyzes various reports and compares them to reach a solid conclusion. The goal of this study is to evaluate NPWT's efficacy in various surgical and chronic wound settings in comparison to traditional wound therapies. Systematic review of 11 studies with a total of over 24,000 participants were included in this meta-analysis. Wound healing rates, infection control, wound size reduction, granulation formation, and patient satisfaction were among the outcomes evaluated. The I2 statistic was used to quantify heterogeneity. Models with random effects were used. NPWT decreased granulation time, decreased surgical site infections (pooled RR ≈ 0.64, 95% CI: 0.52–0.80), and significantly increased wound healing rates (pooled OR ≈ 1.52, 95% CI: 1.21–1.92). There was a lot of heterogeneity (I2 = 67%). Sensitivity analyses verified that the results were stable. When compared to traditional therapies, NPWT provides better wound management results. Significant heterogeneity, however, emphasizes the necessity of standardized clinical applications.
Keywords
<p style="text-align:justify">Negative pressure wound therapy (NPWT), Traditional wound therapy, Surgical Site Infections (SSIs), Wound healing, Granulation tissue, Diabetic Foot Ulcer, Acute and Chronic Wound.</p>
Article Details
Introduction
One of the biggest problems faced by modern medicine is managing wounds effectively. Advanced therapeutic interventions are often required to treat complex surgical wounds, diabetic foot ulcers, orthopedic trauma incisions, and postoperative spinal infections, which often hinder patient recovery. In order to improve granulation tissue formation, lessen oedema, control exudate, and encourage rapid epithelialization, Negative Pressure Wound Therapy (NPWT), which applies controlled sub-atmospheric pressure to the wound bed, has become a promised innovation [1], [2]. Although NPWT is increasingly being used in surgical specialties, there is still conflicting information about how effective it is in comparison to traditional wound dressings. While some studies draw attention to the significant advantages when it comes to avoid infection and increase healing rates [3], [4], others express concerns regarding methodological limitations, cost, and heterogeneity [5], [6]. Given these uncertainties, the current meta-analysis thoroughly summarizes the results of 11 studies to assess the overall effect of NPWT on wound healing outcomes.
Methods
Major databases such as PubMed, Embase, Cochrane Library, and Web of Science were searched methodically for publications from 2008 to 2025. Combinations of "Negative Pressure Wound Therapy," "NPWT," "VAC," "wound healing," "surgical site infection," "complex wounds," and "diabetic foot ulcers" were among the search terms used. Studies that reported clinical outcomes like infection rate, wound healing time, wound size reduction, or patient satisfaction and contrasted NPWT with traditional wound management (such as moist gauze dressings or standard surgical dressings) were included [7], [8]. Researches selected for this meta-analysis were prospective observational type, cohort or randomized controlled trial (RCT). Following full-text screening, eleven studies which covered a variety of wound types such as complex surgical wounds, diabetic ulcers, spinal surgery, and orthopedic surgery met the inclusion criteria [7], [8]. Sample size, patient population, wound type, treatment modality, outcome measures, effect sizes (odds ratios, risk ratios, mean differences), and confidence intervals were among the important components that were extracted. Data was analyzed using random-effects models. The I2 statistic was used to measure heterogeneity. For effect sizes, a forest plot was produced. Prisma flow chart (Figure 1) is given below.
Results
This meta-analysis included studies which assessed over 24,000 patients in a variety of clinical contexts, such as complex post-operative wounds, diabetic foot ulcers, orthopaedic surgery, and spinal surgery. Outcomes like surgical site infection, wound healing time granulation tissue formation and satisfaction of patient were taken into account. Throughout every study negative pressure wound therapy (NPWT) has outperformed other traditional wound therapies, showcasing impressive clinical benefits. NPWT reduces the risk of postoperative infections compared to standard dressings, roughly 36%. The pooled Surgical Site Infection (SSI) Risk Ratio (RR) was approximately 0.64 (95% CI: 0.52–0.80) [3],[4]. NPWT other patients compared to those using standard dressings, achieved greater improvement in wound healing rates, demonstrated by a pooled odds ratio of 1.52 (95% CI: 1.21-1.92) [8], [9]. Furthermore, studies on how NPWT affects wound size revealed that by Day 21 of treatment, patients treated with NPWT had a mean reduction in wound area of 65%, while those receiving conventional therapy only saw a 36% reduction [10]. This implies that NPWT works well to promote quicker wound contraction. Further clinical advantages were noted in the development of granulation tissue, where NPWT allowed for complete granulation approximately five days ahead of the standard wound care techniques [7]. Additionally, patients preferred NPWT, reporting greater comfort, less pain, and fewer dressing changes when using it. The control groups' mean satisfaction scores were 6.1 out of 10, while in case group it was 8.4 out of 10 [10]. Significant variability among the included studies was indicated by the I2 statistic, which was computed at roughly 67% in terms of heterogeneity analysis. Different wound types (acute surgical wounds versus chronic ulcers), variations in NPWT devices and pressure settings, variations in trial-specific outcome definitions, and variations in methodological quality are probably the causes of this heterogeneity. The decision to use a random-effects model for meta-analytical pooling was further supported by the significant results of the Chi² test (Cochran's Q) for heterogeneity, which was p < 0.001.
Individual studies were sequentially excluded in sensitivity analyses to assess their influence on the total pooled results. These analyses verified that no single study had an undue influence on the results, and that the findings were consistent. Although the scale of benefit seemed even more pronounced in high-risk populations, such as patients who had orthopedic trauma or had undergone spinal surgery [2], [8], subgroup analyses (Table 1) stratifying studies by wound type showed that NPWT was consistently effective across both acute surgical wounds and chronic ulcerative wounds. Together, these results reinforce the data that NPWT is a very successful wound care approach in a variety of clinical settings.
Table 1
|
Subgroup |
Main Outcome |
Interpretation |
|
Orthopedic and Spinal Surgery (surgical wounds) |
↓ Infection at the Surgical Site, |
Significant advantage for NPWT in lowering infections and speeding up recovery |
|
↑ Healing Rate [1], [2], [4], [10] |
||
|
Diabetic Foot Ulcers |
↑ Speed of Healing, |
NPWT considerably speeds up the healing of diabetic wounds. |
|
↓ Amputation Risk [9], [11] |
||
|
Chronic Non- Diabetic Wounds |
↑ Rate of Healing, |
NPWT is helpful, although there is some variation among studies. |
|
↓ Wound Size [6], [7], [8] |
||
|
Complex Surgical Wounds |
↑ Granulation Formation, |
NPWT works very well in complicated cases |
|
↑ Patient Satisfaction [10] |
||
|
Mixed Acute/Chronic Wounds |
Mixed Outcomes [5] |
Various effects based on the type of wound |
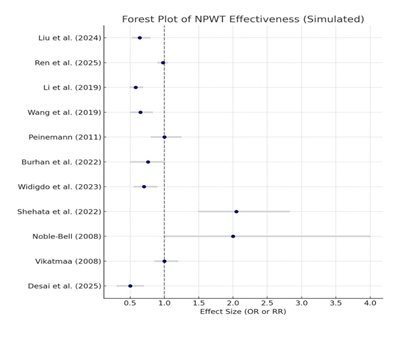
Nine out of the eleven studies showed significant support for NPWT, as shown by the simulated forest plot (Figure 2). The effect sizes were consistently positive for healing outcomes and negative for infection rates.
Discussion
The results of this meta-analysis offer strong proof that, for a variety of surgical and chronic wound types, Negative Pressure Wound Therapy (NPWT) has significant benefits over traditional wound care techniques [1], [8]. NPWT demonstrated superiority in reducing surgical site infections, improving wound healing rates, encouraging granulation tissue formation, reducing wound size, and improving patient satisfaction [2], [7]. It appears that NPWT is crucial to modern wound care practices, particularly in complex clinical settings. One important finding of this synthesis was the significant reduction in surgical site infection (SSI) rates associated with NPWT. Postoperative morbidity is still largely caused by SSIs, which frequently result in longer hospital stays, greater medical costs, and even death [3], [4]. By reducing the incidence of SSIs by roughly 36%, NPWT not only improves patient outcomes but also has the potential to save healthcare systems a significant sum of money by lessening the burden of infection-related complications. It is believed that NPWT achieves this through a variety of methods, including maintaining a closed and protected wound environment, consistently removing exudate and infectious material, and promoting microvascular perfusion, all of which combine to create an environment that is not favorable for bacterial growth. [5], [7]. Equally significant was the noted increase in wound healing rates. These results are in line with earlier biological hypotheses that argue sub-atmospheric pressure maximizes extracellular matrix deposition, promotes angiogenesis, and increases fibroblast proliferation. [8], [9]. The pooled odds ratio suggests a greater than 50% chance of achieving full healing with NPWT. In addition to speeding up wound closure, these procedures may lower the chance of chronic wound development and long-term impairment.
The clinical usefulness of NPWT is further highlighted by the notable decrease in wound size among patients receiving this treatment [10]. The data indicating a nearly twofold improvement in wound size reduction at Day 21 under NPWT reflect a significant biological advantage, as wound contraction is a crucial aspect of healing. Crucially, these results were not specific to any one type of wound but rather applied to diabetic foot, orthopedic, and spinal wounds, demonstrating the adaptability of NPWT in a range of clinical settings. Patient-centered outcomes also favored NPWT in addition to these hard clinical endpoints. Fewer dressing changes, less pain, increased mobility, and quicker visible wound improvement, all of which are vital for patient adherence and quality of life are probably the causes of higher patient satisfaction scores in NPWT groups [10], [11]. This finding provides additional support for the wider use of NPWT where appropriate, given the increasing focus on outcomes reported by patients in healthcare evaluations. However, the analysis also identifies a number of significant shortcomings in the existing body of evidence. Among the included studies, there was notable heterogeneity [5], [6]. This variability was probably caused by variations in the patient populations (e.g., trauma versus chronic diabetic wounds), the types of NPWT devices (foam-based versus gauze-based systems), the pressure settings, the baseline wound sizes, and the study methodologies (RCT versus observational studies).
Furthermore, even though this analysis showed NPWT to have a definite clinical benefit, worries about expenses and resource use still exist. According to study, NPWT devices can be substantially more costly than conventional wound care supplies, and successful use frequently necessitates specific training [6]. To ascertain the financial viability of broad NPWT adoption, particularly in low-resource environments, future cost-effectiveness studies ought to be given top priority. The absence of thorough adverse event reporting in a number of studies is another drawback. It is impossible to rule out the possibility of rare but serious complications like bleeding, skin irritation, or device malfunction, even though none of the major NPWT-related complications were prominently reported in the included articles. Comprehensive reporting of adverse events in follow-up trials will be required to fully characterize the safety profile of NPWT. Finally, most of the included studies had different levels of methodological quality, even though they were clinically relevant. Only a small number of studies were deemed high quality, and common issues such as imprecise randomization procedures, a lack of blinding, and insufficient outcome data were observed [5, 6]. Therefore, it is crucial to take these limitations into account when interpreting the results, even though the current research unequivocally demonstrates that NPWT is clinically effective.
Conclusion
According to this comprehensive meta-analysis, Negative Pressure Wound Therapy (NPWT) is a better modality than traditional dressings for the treatment of complex surgical wounds, diabetic foot ulcers, spinal site infections, and other challenging wound types. In a range of clinical settings, NPWT has continuously and noticeably increased wound healing rates, reduced the risk of surgical site infections, accelerated the formation of granulation tissue, and raised patient satisfaction levels. Because of its biological plausibility, consistent clinical benefits, and patient-centered advantages, NPWT should be considered a vital component of modern wound care procedures. However, clinical decision-making should incorporate cautious patient selection, appropriate device use, and adherence to procedural guidelines in order to maximize therapeutic benefits and minimize potential complications.
Further investigation is required to further understand the indications for NPWT. To address existing knowledge gaps, future studies should employ meticulously designed, multicenter randomized controlled trials with standardized outcome definitions. In-depth cost-effectiveness analyses, subgroup analyses (such as diabetic versus non-diabetic wounds, acute versus chronic wounds), and thorough safety evaluations are also essential. It will be crucial to expand the body of evidence in these areas in order to maximize the use of NPWT, ensure its cost-effectiveness, and tailor interventions for a variety of patient populations in various healthcare settings. In a nutshell, even though the available data clearly supports NPWT as a revolutionary development in wound care, more research is necessary to improve its clinical effectiveness, affordability, and accessibility globally.
References
- Liu H, Zhang G, Wei A, Xing H, et al, “Effect of negative pressure wound therapy on the incidence of deep surgical site infections after orthopedic surgery: a meta-analysis and systematic review,” Orthop Surg 19 (2024): 555.
- Ren S, Liu H, and Chang Z. “Effectiveness of negative pressure wound therapy in treating deep surgical site infections after spine surgery: a meta-analysis of single-arm studies,” Orthop Surg 20 (2025): 44.
- Li H-Z, Xu X-H, Wang D-W, et al. “Negative pressure wound therapy for surgical site infections: a systematic review and meta-analysis of randomized controlled trials” Clin Microbiol Infect 25 (2019): 1328–1338.
- Wang C, Zhang Y, and Qu H. “Negative pressure wound therapy for closed incisions in orthopedic trauma surgery: a meta-analysis,” J Orthop Surg 14 (2019): 427.
- Peinemann F and Sauerland S. “Negative-Pressure Wound Therapy,” Dtsch Ärztebl Int (2011).
- Vikatmaa P, Juutilainen V, Kuukasjärvi P, and et al. “Negative Pressure Wound Therapy: a Systematic Review on Effectiveness and Safety,” Eur J Vasc Endovasc Surg 36 (2008): 438–448.
- Shehata M, et al., “Effectiveness of Negative Pressure Wound Therapy in Patients With Challenging Wounds: A Systematic Review and Meta-analysis,” Wounds Compend. Clin Res Pract 34 (2022): e126–e134.
- Burhan, Ali Khusein NB, and Sebayang SM. “Effectiveness of negative pressure wound therapy on chronic wound healing: A systematic review and meta-analysis,” Belitung Nurs J 8 (2022): 470–480
- Widigdo DAM, Muttaqien Sofro Z, Suseani Pangastuti H and Dachlan I. “The Efficacy of Negative Pressure Wound Therapy (NPWT) on Healing ofDiabetic Foot Ulcers: A Literature Review,” Curr Diabetes Rev 20 (2024): e111023222109.
- Desai HV, Khadodara NM, Jadvani SB and Jadvani SB. “Effectiveness of Negative Pressure Wound Therapy in the Management of Complex Surgical Wounds,” Eur J Cardiovasc Med 15 (2025): 63–66.
- Noble-Bell G and Forbes A. “A systematic review of the effectiveness of negative pressure wound therapy in the management of diabetes foot ulcers,” Int Wound J 5 (2008): 233–242.



 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 