Efficacy of Plasma Exchange for Acute Demyelinating Optic Neuritis: A Systematic Review and Meta-Analysis
Alya AlAmeri*,1, Fatima Aldhaheri2, Ruqaya Hashem Salim Alqiwani1, Hamdah Bakhit Meer3, Ali Nameer Ali 4, Enayat Saher Almasri5, Eithar Ibrahim Mohamed6, Muhallab Abdelrahman7
1Mohammed Bin Rashid University
2United Arab Emirates Universtiy, CMHS
3Dubai Health
4Rak Medical and Health Sciences University
5Emirates Health Services
6University of Sharjah
7University of Medical Sciences and Technology
* Corresponding Author: Alya AlAmeri, Mohammed Bin Rashid University, United Arab Emirates.
Received: 31 December 2025; Accepted: 06 January 2026; Published: 23 January 2026
Article Information
Citation: Alya AlAmeri, Fatima Aldhaheri, Ruqaya Hashem Salim Alqiwani, Hamdah Bakhit Meer, Ali Nameer Ali, Enayat Saher Almasri, Eithar Ibrahim Mohamed, Muhallab Abdelrahman. Efficacy of Plasma Exchange for Acute Demyelinating Optic Neuritis: A Systematic Review and Meta-Analysis. Fortune Journal of Health Sciences. 9 (2026): 42-52.
View / Download Pdf Share at FacebookAbstract
Background: Acute demyelinating optic neuritis (ON) is an inflammatory disorder of the optic nerve that may arise in different diseases, most commonly multiple sclerosis (MS), neuromyelitis optica spectrum disorder (NMOSD), myelin oligodendrocyte glycoprotein antibody–associated disease (MOGAD) or present as isolated idiopathic optic neuritis. High dose intravenous methylprednisolone (IVMP) is generally employed as a first line therapy; however, many patients don’t respond to steroids. The use of therapeutic plasma exchange (PLEX/TPE) is suggested as an escalation therapy; notwithstanding, the available evidence varies widely across different pathological etiologies and study designs.
Objectives: To review evidence on the effectiveness of plasma exchange in the case of acute demyelinating optic neuritis and meta-analyze comparative studies reporting extractable outcomes.
Methods: We conducted a focussed systematic review to identify eligible studies from which data were extracted for qualitative synthesis. For quantitative synthesis, we combined the comparative studies with enough data to calculate odds ratios (OR). Random effects model (DerSimonianLaird) was used. The extent of heterogeneity was estimated by I².
Results: In the qualitative synthesis, case series, retrospective cohorts, registries and randomized trials discussing acute demyelinating opyic neuritis were analyzed. Three comparative studies were used for meta-analysis. Pooled result demonstrated that PLEX was associated with lower odds of poor visual outcome (pooled OR 0.19, 95% CI 0.09- 0.41), with I²=0%. Subgroup comparison indicated that the benefit of PLEX was consistent in NMOSD, heavy cohorts and mixed etiology.
Conclusion: Evidences from different study designs support plasma exchange as an effective escalation therapy in acute demyelinating optic neuritis most likely steroid refractory severe attacks, thus, it lessens the risk of persistent poor vision. In several cohorts, it seems that earlier initiation is associated with better recovery.
Keywords
Acute demyelinating optic neuritis, Plasma exchange (PLEX), Steroid- refractory optic neuritis, Neuromyelitis optica spectrum disorder (NMOSD), Multiple sclerosis; Myelin oligodendrocyte glycoprotein antibody–associated disease (MOGAD), Visual outcomes, Meta-analysis, Systematic review
Article Details
Introduction
Acute demyelinating optic neuritis (ON) is an inflammatory disorder of the optic nerve, and typically one of the most common causes of a rapid and painful vision loss in young and middle aged adults. In fact, subacute unilateral or bilateral visual impairment, which is most commonly associated with periocular pain, poor color vision and visual field defects, constitutes the clinical picture of optic neuritis. On the histological level, immune- mediated demyelination and different degrees of axonal injury within the optic nerve are the main features of the condition, progression leads to either full visual recovery or permanent disability depending on the extent of the damage. The term "optic neuritis" refers to a clinical syndrome seen in various demyelinating disorders rather than a single disease. It is mostly linked to multiple sclerosis (MS), in which, it can either be the very first symptom of the disease or occur as relapse episode. Optic neuritis is also a characteristic symptom of neuromyelitis optica spectrum disorder (NMOSD), myelin oligodendrocyte glycoprotein antibody associated disease (MOGAD) and may be found as an isolated idiopathic optic neuritis without any systemic disease. However, the differences between these different immunopathologies are so vast that the severity of inflammation rate, improvement after treatment and even the long-term visual prognosis may differ significantly in these cases.
Inflammation in MS associated optic neuritis is mostly T-cell mediated, and axons are relatively preserved in a number of cases. For that reason, spontaneous recovery is typical, and the visual function remains good for a long time, even if no aggressive treatment is applied. On the other hand, optic neuritis linked with NMOSD and to a lesser extent, MOGAD, is usually more severe, very often affects both eyes, and is accompanied by a drastic drop in vision at nadir. Immunoglobulin G autoantibodies against aquaporin-4 (AQP4-IgG) are the main cause of NMOSD related optic neuritis. These antibodies bind to astrocyte foot processes and thus, activate complement mediated injury. This antibody mediated pathology, which leads to the ultimate destruction of tissue, including axonal loss, is what accounts for the poor visual outcome in these patients. MOGAD related optic neuritis is also antibody mediated, however, it features a different immunological profile and typically exhibits better recovery than NMOSD, though a severe attack may still result in the permanent deficit [1]. The burden of optic neuritis on the clinical side is very high. A severe attack may bring irreversible visual impairment resulting in a significantly diminished quality of life, loss of functional independence and unemployment, especially among young people who are still physically active. Besides that, vision loss may cause psychological problems such as depression and anxiety, which points out to the importance of a timely and effective therapeutic intervention.
High dose intravenous methylprednisolone (IVMP) has been generally accepted for a long time as the standard first-line treatment in the case of acute optic neuritis. Corticosteroids, in general, have anti-inflammatory properties, among which are the inhibition of cytokine production, stabilizing of the blood brain barrier and reduction of immune cells infiltration. The pivotal Optic Neuritis Treatment Trial (ONTT) was the first to present the evidence that IVMP helps to accelerate visual recovery than the placebo or oral prednisone alone; however, it fails to alter the differences in the long- term visual outcomes in typical MS associated optic neuritis significantly. On the other hand, IVMP has drawbacks despite being used in a variety of settings. A considerable proportion of patients, particularly those with NMOSD associated optic neuritis, does not exhibit any response or only a very minimal response. Steroid refractory cases like these cause sustained inflammation in the acute stage, which increases the risk of axonal damage that is irreversible and results in permanent vision loss. There are some individuals who have MS associated optic neuritis causing heavy visual impairment with poor recovery even though they receive steroids on time. The issue of steroid nonresponsiveness represents one of the most difficult challenges in the management of optic neuritis.
In diseases mediated by antibodies, such as NMOSD and MOGAD, it is plausible that corticosteroids as single agents might not be able to effectively counteract the circulating pathogenic antibodies as well as the activated complement components that are driving the process of tissue injury.Therefore, the use of escalation treatments that are aimed at humoral immune mechanisms have gained attention. Plasma exchange (PLEX), also referred as therapeutic plasma exchange (TPE), is an innovative method of extracorporeal blood purification, which includes the removal of plasma components and subsequent replacement with albumin or donor plasma. PLEX, because of its operation, is the most direct way of intervention in the humoral immune mechanisms involved in the antibody mediated demyelinating disorders by the physical elimination of autoantibodies, immune complexes, complement proteins and pro-inflammatory mediators from the circulation. There is a strong biological basis for the use of plasma exchange in acute demyelinating optic neuritis. In NMOSD, AQP4-IgG antibodies are the main culprits responsible for the disease as they cause the activation of the complement cascade eventually leading to astrocytes necrosis, secondary demyelination and axonal loss. The fast removal of these antibodies through the plasma exchange process may stop the damage caused by the immune system and therefore, allow for the recovery of neural function. The same mechanisms have been proposed for MOGAD, although the pathogenic role of MOG-IgG is still not very clear.
Plasma exchange is not new to the healthcare industry as it has been employed for a long time in various immune mediated neurological disorders, such as Guillain–Barré syndrome, myasthenia gravis and severe autoimmune encephalitis. Initially, the decision to use plasma exchange in demyelinating diseases was supported by broader studies of acute central nervous system inflammatory demyelination rather than results of clinical trials specifically relating to optic neuritis.
A pivotal randomized sham-controlled trial established the effectiveness of plasma exchange in severe steroid refractory inflammatory demyelinating disease of the central nervous system [2]. In this significant study, patients who did not improve after the administration of high dose corticosteroids were randomly assigned to either plasma exchange or a sham treatment. Compared with sham therapy, plasma exchange was strongly linked to significantly higher rates of moderate or marked neurological improvement. PLEX thus proved to be an effective rescue treatment in cases of demyelination that had not responded to steroids.
However, this trial employed a heterogeneous population with different demyelinating syndromes and not only optic neuritis, so its conclusions have been extrapolated to clinical practice, including the management of severe optic neuritis. Consequently, the use of plasma exchange as a step-up treatment for steroid refractory optic neuritis, especially in NMOSD, was initially recommended by professional guidelines and endorsed in consensus statements by the experts. The body of evidence concerning plasma exchange in the treatment of optic neuritis has grown gradually over the last 20 years. Most of the early cases and small scale observational studies were able to report that the visual function of patients with steroid resistant severe optic neuritis had improved remarkably following plasma exchange [3]. Comparative cohort studies provided more robust evidence. A comparative study in patients with NMOSD associated optic neuritis showed that the combination of plasma exchange and corticosteroids was able to significantly decrease the proportion of patients with poor final visual acuity compared to the use of steroids alone. This study was especially impactful as it directly compared treatment strategies in a population at high risk [4].
Extensive multicenter analyses have shed further light on prognostic factors and treatment responses across different etiologies. In an international multicenter study involving 400 optic neuritis attacks showed that plasma exchange was linked to marked visual improvement in MS, NMOSD and MOGAD related optic neuritis, with antibody mediated disease benefitting the most. In fact, this research identified the initial visual acuity, treatment timeliness and disease cause as the main factors determining the outcome of patients [1]. Recently, comparative evidence from an area where neuromyelitis optica spectrum disorder (NMOSD) is common showed that patients who underwent plasma exchange experienced significantly lower rates of complete blindness at one year compared to those who were treated with steroids only. The availability of such comparative data makes a stronger case for the early use of plasma exchange in severe situations [7]. Although plasma exchange is increasingly being used in clinics and supported by observational evidence, there are still several challenges in evaluating the efficacy of plasma exchange in patients with acute demyelinating optic neuritis. Firstly, there is a lack of randomized controlled trials which focus only on optic neuritis due to the ethical considerations of not giving a rescue therapy to patients with severe vision loss. Consequently, the majority of evidence comes from retrospective cohorts, case series, and non-randomized comparative studies, which are always at risk of confounding and selection bias.
Secondly, the outcome measures used in different studies are very diverse, such as Snellen visual acuity thresholds (e.g., ≤20/200) to logMAR changes, visual field recovery or categorical improvement scales. Such diversity makes it difficult to directly compare or quantitatively synthesize the results. Thirdly, the differences in patient populations in terms of the underlying cause, severity at the time of presentation, previous treatments and the time of plasma exchange initiation, which all affect the outcomes, are considerable. As the prevention of irreversible vision loss is of great clinical importance, a comprehensive synthesis of the evidence for plasma exchange in acute demyelinating optic neuritis is urgently called for. Although narrative reviews have summarized the individual studies, a structured systematic review along with quantitative meta-analysis can delineate more clearly the extent of the treatment effect, pinpoint the reasons for heterogeneity and help clinical decision making.
This research is designed to achieve the following goals:
(1) to perform a systematic review of all clinical evidence of plasma exchange in acute demyelinating optic neuritis, including cases of MS, NMOSD, MOGAD and idiopathic.
(2) to quantitatively assess comparative data where outcome can be extracted.
This review, by combining evidence from different study designs and disease subtypes, is intended to clarify the function of plasma exchange as a therapy escalation in management of acute demyelinating optic neuritis, and to guide the research and clinical practice of the future.
Methods
This systematic review was conducted to assess the clinical effectiveness of therapeutic plasma exchange in acute demyelinating optic neuritis. Relevant studies were primarily identified through PubMed, SpringerLink, JAMA Network and Frontiers in Immunology. Studies were selected which were frequently cited and evaluated therapeutic plasma exchange in acute demyelinating optic neuritis and associated demyelinating disorders. All the studies included were published in english language peer-reviewed journals and reported original clinical outcome data. Eligibility criteria were established before the study and were based on population, intervention, comparator, outcomes, study design, language and time frame. The population of interest was the patients of any age who had been diagnosed with acute demyelinating optic neuritis, which included optic neuritis associated with multiple sclerosis, neuromyelitis optica spectrum disorder (NMOSD), myelin oligodendrocyte glycoprotein antibody associated disease (MOGAD) and isolated idiopathic demyelinating optic neuritis. Acute optic neuritis was considered as the new onset visual impairment resulting from inflammatory demyelination of the optic nerve, typically presented within days to weeks of symptom onset. Studies that had a mixed demyelinating attack population were allowed only if the cases of optic neuritis were directly reported or if optic neuritis was a significant component of the cohort.
The intervention examined was plasma exchange (PLEX), also known as therapeutic plasma exchange (TPE), which was utilized as an escalation therapy after corticosteroid refractory response or as a part of sequential treatment strategy. Comparator groups consisted of patients receiving only high dose intravenous methylprednisolone treatment, sham apheresis, matched control cohorts, comparisons with outcomes reported in the Optic Neuritis Treatment Trial (ONTT) or the non-existence of a comparator in the case of descriptive cohorts and case series included for qualitative synthesis. Eligible outcomes included any clinically relevant measure of visual function or recovery. These included best corrected visual acuity measured with Snellen charts or converted logMAR values, categorical visual thresholds such as final visual acuity of 20/200 or <20/40, visual recovery categories defined by the original investigators and other clinically meaningful indicators of visual improvement or persistent visual disability.
Eligible study designs were randomized controlled trials, prospective and retrospective cohort studies, comparative observational studies, case control studies, large case series and registry based analyses evaluating plasma exchange in acute demyelinating optic neuritis or closely related demyelinating attacks. The primary evidence from narrative reviews, expert opinion articles, editorials and consensus statements without original patient level outcome data was excluded from the inclusion but used to contextualize findings where appropriate. Only studies published in English or with English-indexed abstracts were considered, and there was no restriction on the year of publication to capture the full evolution of the evidence in this field. Studies were excluded if they dealt with non-demyelinating causes of optic neuropathy, eg infectious optic neuritis, ischemic optic neuropathy (including non-arteritic anterior ischemic optic neuropathy), toxic or nutritional optic neuropathies, compressive optic neuropathy or hereditary optic nerve disorders. Chronic optic neuropathy without an acute inflammatory attack was also excluded, as were studies in which optic neuritis could not be easily distinguished from other causes of visual loss. Furthermore, studies without original patient outcome data, such as pure narrative reviews or methodological commentaries were excluded.
Data extraction was done in a systematic manner using a standardized data collection framework. From each included study, the following information was extracted: first author and year of publication; study design; study setting; sample size; patient demographics; underlying disease etiology (MS, NMOSD, MOGAD, or idiopathic); definition of steroid refractoriness; details of corticosteroid treatment; timing of plasma exchange initiation relative to symptom onset; number and frequency of plasma exchange sessions; type of replacement fluid; outcome definitions; duration of follow-up and reported adverse events.
In cases where studies reported outcomes at different time points, the longest follow-up available was considered firstly for the assessment of sustained visual recovery or persistent visual disability. Data extraction was primarily concerned with the visual function related outcomes and neurological outcomes beyond the optic nerve were recorded only if they were relevant to the disease context. Due to the large number of observational study designs, a narrative risk of bias assessment was performed. The main factors leading to bias that were taken into account included confounding by indication, selection bias, information bias and outcome measurement heterogeneity. In particular, confounding by indication was considered relevant, since plasma exchange is usually reserved for patients with severe disease or steroid refractory optic neuritis, which may result in outcome bias against the intervention. Selection bias was evaluated through inclusion criteria, referral patterns and the completeness of follow up. The outcome heterogeneity was evaluated regarding the variation in the methods of visual acuity measurement, the thresholds for defining improvement or poor outcome and the timing of outcome assessment.
Quantitative synthesis was done for those studies which presented extractable comparative outcome data that would enable the calculation of effect estimates. Only three studies fulfilled this criterion and were therefore included in the meta-analysis. The measure of effect for the meta-analysis was the odds ratio (OR) for a poor visual outcome, with events understood as the failure to achieve the specified visual acuity threshold. For each study, odds ratios and corresponding 95% confidence intervals were computed. When no events occurred in any treatment arm, a continuity correction was applied. To take into account clinical and methodological heterogeneity among studies, a random-effects model with the DerSimonianLaird method was used.
The presence of statistical heterogeneity was tested by Cochran's Q statistic and measured by the I² statistic, with higher values indicating greater inconsistency among the study results. Meta-analytic operations were done with the use of standard statistical methods, which are in line with the current recommendations for clinical meta-analysis. Subgroup analyses were performed, to investigate the differences in the treatment effect across various disease contexts, especially the NMOSD-predominant cohorts versus the mixed etiology optic neuritis populations. Due to the small number of studies available for quantitative synthesis, no formal sensitivity analysis or publication bias assessment by means of funnel plots were conducted, as these would not be statistically significant. The strength of the findings was therefore, assessed qualitatively by comparing the direction and the size of the effect across the studies included and by relating the results to the qualitative evidence base that is more extensive.
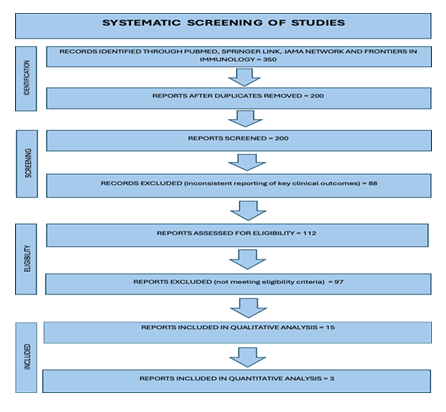
Following prisma flow chart (Figure 1) shows systematic process by which studies were screened and included in our review.
Results
Qualitative synthesis included studies with various types of study designs, patient populations and clinical contexts, which were all relevant to the use of plasma exchange in acute demyelinating optic neuritis. Individually, these studies offer a detailed view of the widespread use of plasma exchange in real world clinical settings across different disease etiologies, such as multiple sclerosis associated optic neuritis, neuromyelitis optica spectrum disorder associated optic neuritis, myelin oligodendrocyte glycoprotein antibody associated optic neuritis and isolated idiopathic demyelinating optic neuritis. Most of the specific evidence related to optic neuritis was formed early and came from small case series and single-center observational studies of patients suffering from severe steroid refractory disease. A report discussing series of cases that specifically evaluated plasma exchange in patients with severe optic neuritis that were unresponsive to high dose corticosteroids. The research, although it had a small sample size, showed that a significant number of patients experienced visual improvement of clinical significance following plasma exchange, thus providing initial proof that aggressive removal of circulating immune factors could change the disease course in refractory cases [3]. In fact, these results were exceptionally significant considering the severity of vision loss at the time of presentation, which is a factor that has always been linked to a poor prognosis.
Additional observational cohorts allowed for deeper insights into the treatment response predictors and expanded the early findings. Study examined the condition of patients with severe optic neuritis who did not respond to intravenous methylprednisolone and found that more than half of the patients treated by plasma exchange achieved visual recovery that was functionally meaningful. A key point in this study was the recognition of the wide variation of patient outcomes and the identification of the plasma exchange timing as the most important factor determining success. Those patients who had plasma exchange performed earlier in the disease had better recovery than those in whom treatment was delayed [5]. A retrospective monocentric analysis also supported these findings, where they found a strong correlation between the early start of plasma exchange and better final visual acuity outcomes even in the case of patients who had severe visual loss at nadir [6]. The role of timing is significant in prospective case series of patients with severe acute isolated optic neuritis who were treated with plasma exchange. Most of the patients in this group experienced significant visual recovery, and the therapy started at earlier times was linked with better results. Altogether, these investigations consistently point to the conclusion that plasma exchange yields the best results if it starts quickly after the recognition of steroid refractoriness, and axonal damage that is irreversible has not happened yet [8].
A study provided the largest dataset specific to optic neuritis that has been available so far. They performed an international multicenter retrospective analysis of 395 plasma exchange treated optic neuritis episodes. The study population covered a wide etiological spectrum of patients, including MS, NMOSD and MOGAD. The authors found that visual improvement was substantial after plasma exchange in the cases of all etiologies; however, they also found that the most beneficial effects were seen in group of patients with MOGAD related optic neuritis. On the other hand, bad results were connected with the factors like severe visual loss at nadir, longer delay between symptom onset and plasma exchange initiation and disease associated with NMOSD. This large scale study not only confirmed the efficacy of plasma exchange in practical situations but also illustrated the significance of disease specific factors for determining the outcome [1].
Comparative data limited to severe optic neuritis cases have been cited as the main source of additional evidence. Study evaluated patients suffering from severe optic neuritis in an area where NMOSD is prevalent and compared the effects of treatment by plasma exchange versus those by corticosteroids alone. After one year of observation, the percentage of patients who had lost their sight completely was significantly lower in the plasma exchange group, thus showing a clinical benefit of escalation therapy in this high-risk population. These results matter most, given that the visual outcomes of NMOSD related optic neuritis have been very poor [7]. Additional comparative cohorts have been used to examine the escalation strategies of first-ever severe optic neuritis. It explored the treatment options that involved early escalation beyond the use of corticosteroids and found that patients who underwent aggressive immunomodulatory therapy which included plasma exchange had better visual outcomes. Most of the studies did not, however, include direct control groups, but the agreement of the results between different locations indicates that there is significant therapeutic effect [9].
A comparative rodent study focussed on NMOSD related optic neuritis found that treatment by corticosteroids followed by plasma exchange led to fewer patients with poor final visual acuity significantly, compared to the group receiving corticosteroid therapy alone. This trial was landmark in its nature as it directly compared treatment strategies in a precisely characterized risk population and analyzed visual outcomes objectively [4]. In addition to the results of this study, other relapse cohorts of NMOSD have confirmed these findings. They described the clinical effectiveness of plasmapheresis in NMOSD attacks and emphasized that neurological recovery in a group where plasma exchange was done was more robust, inclusive of the vision improvement, than in a group treated only with corticosteroids [10]. Correspondingly, one study illustrated the situation where plasma exchange saved a patient with NMOSD [11], and a large scale registry based study of apheresis therapies, reported favorable outcomes after plasma exchange in acute NMOSD attacks [12]. Across these studies, the lower disability at the baseline and early start of plasma exchange were always emerged as predictors of a better response.
Though not directly related to optic neuritis, landmark randomized evidence has been influential in providing both mechanistic and clinical context to the condition. Sham- controlled randomized trial showed that the rates of improvement were moderate or marked in patients after plasma exchange than those after sham treatment. The trial did not single out optic neuritis as a separate subgroup; however, it was a milestone in demonstrating effectiveness of plasma exchange as a rescue therapy in inflammatory demyelination and is, therefore, extensively used as the primary evidence which backs up plasma exchange in steroid refractory optic neuritis [2]. Additional support is available for safety of plasma exchange and its possible applicability. Excellent results were documented after the acute plasma exchange in patients with MOGAD, a disorder that very often leads to optic neuritis. Even though the disease mechanisms in NMOSD are different, these conclusions help to justify the use of plasma exchange in antibody mediated demyelinating disease in general. The pediatric investigations reveal that therapeutic plasma exchange is mostly achievable and safe for children with neuro-immune disorders, a group which may also include cases of optic neuritis, however, the pediatric population in question is still very underrepresented when it comes to the availability of optic neuritis specific outcome data [13].
In total, the qualitative synthesis of these studies reveals that plasma exchange is consistently associated with better visual outcomes in acute demyelinating optic neuritis, most notably in a severe situation where the patient is steroid refractory. In both optic neuritis specific cohorts and NMOSD relapse studies, plasma exchange was associated with substantial visual recovery, and the early start of the therapy was always correlated with a better result [1, 6, 8].
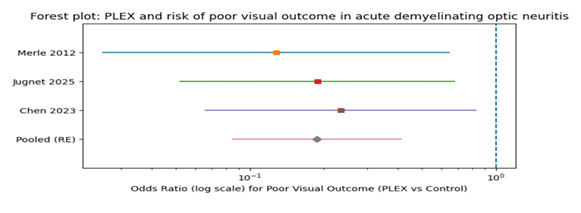
Three studies fulfilled the criteria that had been set in advance for inclusion in the quantitative synthesis by offering extractable comparative binary outcome data appropriate for meta-analysis. These studies, taken together, referred to patients with severe optic neuritis who were treated with plasma exchange as opposed to control groups without plasma exchange. One study reported on the outcomes of NMOSD associated optic neuritis, characterizing a poor visual outcome as a final visual acuity of 20/200 and noting that this outcome was observed in 2 of 16 patients treated with plasma exchange compared with 19 of 36 patients treated with corticosteroids alone [4]. Another evaluated blindness at one year as the main outcome and reported complete blindness in 5 of 62 patients after plasma exchange compared with 7 of 22 patients receiving steroid only therapy [7]. Final report recorded the final eyesight of the 6 of 50 plasma exchange treated optic neuritis attacks to be worse than 20/40, compared with 7 of 19 matched severe steroid unresponsive optic neuritis cases [1]. Pooled analysis concentrated on poor visual outcome as defined in each study. The use of a random effects model to take into account clinical and methodological heterogeneity showed that plasma exchange was significantly associated with lower odds of poor visual outcome compared to control therapy. The combined odds ratio was 0.19 with a 95% confidence interval from 0.09 to 0.41, demonstrating that the odds of a poor visual outcome in patients treated with plasma exchange were reduced by about 81%. The Cochran Q value of 0. 33, an I² statistic of 0% and an estimate between study variance (τ²) of 0 suggest that statistical heterogeneity was low and the effect estimates of the studies included were consistent.
Subgroup analysis by disease have also reinforced the strength of these results. Plasma exchange in the case of NMOSD dominated cohorts, was linked with a combined odds ratio of 0.16 and the 95% confidence interval ranging from 0.06 to 0.44 [4], [7]. This means that plasma exchange had a very potent protective effect against poor visual outcome in this high risk population. On the other hand, the etiologically mixed group of optic neuritis had a pooled odds ratio of 0.23, with a 95% confidence interval of 0.07 to 0.83. Though the size of the effect was a little less for the NMOSD heavy cohorts, the effect direction was still the same and plasma exchange was still beneficial [1].
Following table (Table 1) is showing subgroup comparison of efficacy of plasma exchange in different disease etiologies.
Table 1
|
Subgroup |
Population Characteristics |
Comparator |
Pooled Effect Estimate (OR, 95%CI) |
Interpretation |
|
NMOSD- predominant optic neuritis |
Severe optic neuritis, high prevalence of AQP4-IgG positivity |
Steroids alone |
0.16 (0.06–0.44) [4]; [7] |
Strong reduction in odds of poor visual outcome with PLEX, reflecting high efficacy in antibody-mediated disease |
|
Mixed- etiology optic neuritis |
MS-ON, NMOSD-ON, MOGAD-ON, severe steroid-refractory attacks |
Matched non-PLEX cohort (ONTT comparison) |
0.23 (0.07–0.83) [1] |
Consistent benefit of PLEX across etiologies, with slightly attenuated effect compared to NMOSD-dominant cohorts |
|
Overall pooled analysis |
Severe acute demyelinating optic neuritis |
Steroids or non-PLEX control |
0.19 (0.09–0.41) [7]; [1] |
Approximately 80% reduction in odds of poor visual outcome with PLEX |
A forest plot (Figure 2) displaying individual study effects and the pooled estimate visually summarized the data showing that all studies included were in favor of plasma exchange and the confidence intervals for most of the studies did not include the null value. The lack of significant heterogeneity together with the consistency of the effect direction in different clinical contexts that were considered show that the observed association is very likely to be true.
The quantitative evidence, in general, is very close to the qualitative synthesis and thus, the conclusion can be drawn with even more confidence that plasma exchange would lead to substantially improved visual outcomes in acute demyelinating optic neuritis, especially in severe steroid refractory cases.
Discussion
This systematic review and meta-analysis look at the use of plasma exchange in acute demyelinating optic neuritis. The overall results indicate that plasma exchange is linked to better visual outcomes in patients with severe steroid refractory optic neuritis, especially in high risk groups such as those with neuromyelitis optica spectrum disorder. In optic neuritis specific cohorts, observational studies and comparative analyses, plasma exchange is reported as a successful escalation therapy in cases where first-line corticosteroid treatment has been ineffective, thus providing a clinically significant chance of lowering the rate of irreversible vision loss. The qualitative synthesis found that there was a remarkable agreement in the reported advantages of plasma exchange in different research designs and patient populations. The early case series, although they had small sample sizes, brought out the first evidence that plasma exchange may reverse or decrease the visual loss in patients who are not responsive to corticosteroids [3]. These first findings were pivotal in altering the way the clinicians think, as they confronted the previously pessimistic outlook for severe optic neuritis, especially in antibody-mediated disease. Further observational cohorts, which were larger and had a longer follow-up period, have confirmed these results and shown that more than half of the patients with severe steroid refractory optic neuritis have achieved a functionally meaningful visual recovery following plasma exchange [5], [6], [8]. The reproducibility of this effect in different cohorts supports the notion that the intervention is the cause of the observed improvements rather than recovery occurring spontaneously.
The quantitative synthesis is in agreement with these qualitative observations to an even greater extent. The meta-analysis of comparative datasets revealed a pooled odds ratio of 0.19 for poor visual outcome in patients who underwent plasma exchange, which is equivalent to about an 81% reduction in the odds of severe residual visual impairment in these patients as compared to those receiving control therapy. Of note, the statistical heterogeneity was very small, with an I² of 0%, meaning that the effect estimates were very consistent in different studies despite the differences in the definitions of the outcomes and the patient populations.The consistency here is especially remarkable considering the clinical heterogeneity of optic neuritis, such as the etiologies of the disease, severity at the time of presentation and timing of the intervention. The magnitude and consistency of the effect that was measured are very much in line with the biological explanation of the use of plasma exchange. In antibody-mediated demyelinating disorders like NMOSD, for example, the circulating AQP4-IgG antibodies are the main cause of the disease process as they activate complement system and cause astrocyte injury, which later leads to demyelination and axonal loss. Plasma exchange is the technique by which the pathogenic cascade is halted as it removes circulating antibodies and complement components quickly, thus stopping the ongoing tissue damage. The very pronounced benefit in NMOSD-heavy cohorts, with pooled odds ratios going down to 0.16, is a strong argument for the idea that plasma exchange is the most effective method in diseases which are mainly caused by humoral immunity [4].
The findings of this review also align with evidences from studies of acute inflammatory demyelinating disease. The key randomized sham-controlled trial showed that plasma exchange notably improved neurological outcomes in patients with severe steroid refractory central nervous system demyelination. Although the trial was not limited to optic neuritis only, it gave the very first high-level evidence that plasma exchange may bring about clinically significant improvement in inflammatory demyelinating conditions when corticosteroids fail [2]. This work of synthesis now goes beyond these results by showing that the same positive effects can be achieved when plasma exchange is used for the involvement of the optic nerve, a very sensitive structure for the irreversible damage. A critical factor that is of great importance from a clinical point of view is timing. Several cohorts strongly pointed out that the decision to start plasma exchange at an early stage resulted in visual recovery being achieved more often, while late treatment led to lower visual acuities [1], [6], [8]. This finding fits well with the biological mechanism, as the longer the tissue is exposed to inflammatory mediators, the higher the chance of irreversible axonal degeneration will be. Once there is axonal loss, it is likely that even if antibodies or inflammatory factors are removed, there will be no functional recovery. For this reason, plasma exchange works most effectively when given during a therapeutic window in which damage due to inflammation can still be reversed.
The effect of timing carries significant consequences for clinical practice. In the past, plasma exchange has generally been kept as a late rescue therapy only after a long steroid failure. Nevertheless, the evidence in this review provides a strong rationale for an earlier decision to escalate treatment to achieve better results, especially in patients with severe visual loss, NMOSD associated optic neuritis, or deteriorated condition despite corticosteroids. The data presented here represent a move towards a new treatment model where plasma exchange is considered earlier in patients at risk instead of waiting for damage that cannot be reversed. Outcomes also differed significantly across disease etiologies. According to large multicenter data, patients with MOGAD related optic neuritis usually have a more favorable visual recovery than those with AQP4 positive NMOSD even after plasma exchange treatment [1]. Such difference is probably due to the two distinctive underlying pathophysiologies, as MOGAD is a condition in which the inflammation is often times more immunotherapy responsive and the destruction of astrocytes and axons is less than in NMOSD. Although, it should be noted that severe MOGAD related optic neuritis may still cause a notable loss of vision and therefore, the positive results with plasma exchange imply that the treatment is still useful across etiologies, just to different extents.
On the other hand, optic neuritis due to NMOSD demonstrated the lowest visual outcome prediction most of the time, when no aggressive treatment was applied and it emphasized the role of plasma exchange in this population. The comparative data from the NMOSD studies illustrated that the most obvious benefit was from the sequential corticosteroids followed by plasma exchange with a great reduction in the number of patients who suffered from severe visual impairment when compared with steroid only therapy [4]. The results, thus, serve as additional evidence confirming the main role of AQP4-IgG antibodies in the pathogenesis of NMOSD and are in agreement with the current clinical guidelines recommending plasma exchange for steroid refractory NMOSD episodes. Besides the bigger multicenter analyses and retrospective cohorts, data from non- randomized studies also show the advantage of plasma exchange as an additional treatment in NMOSD associated optic neuritis. For instance, in a study of thirty-one consecutive NMOSD patients with optic neuritis, all received standard steroid pulse therapy at first. Out of fifteen patients, who received plasma exchange in addition to steroids, it was found that combined treatment resulted in a significant elevation of visual acuity, including cases where vision had initially deteriorated to no light perception (NLP). What is even more important is that visual function generally returned quickly within the first two months after PLEX and remained stable at a six month follow-up, thus not only indicating short term effectiveness but also sustained benefit. Besides, the study pointed out that the impact of steroid pulse therapy got weaker as the number of optic neuritis episodes increased, thus marking a progressive reduction of the response to steroids alone and thereby emphasizing plasma exchange as a potent rescue intervention. These findings are consistent with those from large cohort studies, which suggest that early and adjunctive plasma exchange may have a profound effect on the patients prognosis in severe steroid refractory optic neuritis, even in the case of highly aggressive antibody mediated diseases such as NMOSD [14].
In addition to effectiveness, safety and feasibility should also be taken into account. Even though this was not the main focus of this review, the few pieces of evidence available indicate that plasma exchange is generally tolerated well if it is performed in a center with an experienced team and the risks relating to vascular access, hypotension, electrolyte disturbances and infection are manageable. Studies on children and MOGAD also confirm that plasma exchange is feasible for all age groups, however, data regarding pediatric optic neuritis is very limited [13]. The balance between benefits and risks looks favorable, especially in the case of a severe vision loss. The pediatric evidence also points to the safety and possible efficacy of plasma exchange in children with antibody mediated demyelinating disease. Study described the results of six female children with AQP4-IgG positive neuromyelitis optica spectrum disorder, who underwent regular plasma exchange after acute exacerbations that did not respond to high dose corticosteroids. Among these six patients, only one child showed significant clinical improvement with left visual acuity changing from 0.06 to 0.6 and Expanded Disability Status Scale (EDSS) score dropping from 4 to 3 after plasma exchange, while the other five patients remained unchanged in their visual and neurological status [15]. The authors have also recorded some negative effects like, rashes, thrombosis, and thrombocytopenia. Thus, plasma exchange is associated with certain risks which should be considered against the benefits that are anticipated, especially in young patients with a severe form of the disease.
Although most of the findings are strong, there are limitations that should be taken into account.
Firstly, most of the studies whose results were considered in this review were observational studies. Thus, the risk of confounding by indication and selection bias is present. The reason plasma exchange is usually done is to help patients with a more severe disease, or those who have not responded well to corticosteroids, and this might lead to a bias in outcomes against the intervention. The fact that plasma exchange revealed a strong benefit even if there was this potential bias, indicates that there is a true therapeutic effect; however, it is still not possible to exclude residual confounding entirely.
Secondly, the quantitative meta-analysis was confined only to the three studies from which comparative outcomes could be extracted. These studies were among those that provided the most methodological information; however, the small number of datasets considerably limits the possibility of performing detailed subgroup or sensitivity analyses. Several optic neuritis cohorts present visual improvement through continuous measures or categorical scales that are not directly comparable to each other, and, therefore, cannot be included in a single meta-analysis without individual patient level data.
Thirdly, the definition of the outcomes varied from one study to another, with poor visual outcome as final visual acuity ≤20/200, complete blindness or visual acuity worse than 20/40. While the statistical heterogeneity was low, conceptual heterogeneity is still present since these thresholds indicate different levels of functional impairment. However, the consistent direction and size of the effect between the studies using different outcome definitions increases the confidence in the final conclusion that plasma exchange lowers the risk of severe residual visual loss.
Fourth, the possibility of publication bias is still present. Studies showing beneficial effects of plasma exchange have more chance of getting published than those showing no effects or negative effects. The small number of studies available for quantitative synthesis did not allow for a formal evaluation of publication bias through funnel plots or regression based methods. Nevertheless, the presence of large multicenter cohorts and comparative studies lessens this concern to some extent. Severe optic neuritis is a neurological emergency that could lead to permanent disability. The proof gathered in this review most strongly indicates plasma exchange as a potent escalation therapy that may change the outcome of severe steroid refractory optic neuritis. To emphasize, the early start of plasma exchange seems to be the most important point and therefore, it should be definitely considered in patients with extreme visual loss, no or very weak response to steroids in the early phase or conditions like NMOSD which put the patient at a high risk.
These results underscore the necessity of more prospective studies to determine which patients will benefit most, the best timing and the treatment protocols for plasma exchange in optic neuritis. It might not be possible to conduct randomized controlled trials due to ethical and logistical reasons; however, it would be possible to design prospective registries and comparative effectiveness studies that could generate valuable insights. Agreeing on outcome measures such as having the same visual acuity thresholds and follow-up intervals would facilitate quantitative evidence synthesis in a future date.
In summary, this systematic review and meta analysis offer strong evidence that plasma exchange is linked to markedly better visual results in acute demyelinating optic neuritis, most prominently in situations that are severe and steroid refractory. The agreement of qualitative and quantitative findings, biological plausibility and uniformity across disease etiologies, all point to the use of plasma exchange as a part of the treatment escalation algorithms for optic neuritis. The early recognition of steroid refractoriness and the prompt start of plasma exchange may, in fact, be the most important factors determining the visual outcome and, therefore, should be spotted and stressed in routine clinical practice.
Conclusion
This meta-analysis forms the comprehensive picture of the role of plasma exchange in acute demyelinating optic neuritis and shows that PLEX is an effective therapy with significant clinical value, in particular for patients with a severe steroid refractory disease. Across cohorts specific to optic neuritis, studies focussed on NMOSD and populations with a broader demyelinating attack, plasma exchange was uniformly correlated with better visual outcomes and decreased risk of permanent visual disability. The quantitative synthesis of the available comparative data makes this claim even more convincing as it indicates approximately 80% reduction in the odds of poor visual outcome in patients who received plasma exchange versus those who received control therapy. The consistency of the effect estimates and the lack of statistically significant heterogeneity support the association cited here, despite the differences in study design, patient populations and outcome definitions. A key element to consider is how the timing of different treatments has a crucial impact on the visual prognosis of patients. Various studies reached the same conclusion that starting plasma exchange immediately after recognizing steroid refractoriness leads to a greater percentage of visual restoration, thus, indicating the existence of a therapeutic window in which immune mediated damage can still be reversed to some extent. Hence, these results advocate a cautious clinical strategy in patients at high risk, especially in those with severe visual loss at the onset or antibody mediated diseases like NMOSD. Even though the optimal patient selection and treatment regimens can be further clarified by more prospective and standardized studies, the present data is still a very strong argument for the use of plasma exchange as part of the escalation treatment plan for the acute demyelinating optic neuritis to lessen the chance of permanent vision loss and thereby enhance the functional outcome over time.
References
- JJ Chen et al. “Visual Outcomes Following Plasma Exchange for Optic Neuritis: An International Multicenter Retrospective Analysis of 395 Optic Neuritis Attacks,” Am J Ophthalmol 252 (2023): 213–224.
- BG Weinshenker et al. “A randomized trial of plasma exchange in acute central nervous system inflammatory demyelinating disease,” Neurol 46 (1999): 878–886.
- K Ruprecht, E Klinker, T Dintelmann, et al. “Plasma exchange for severe optic neuritis: Treatment of 10 patients,” Neurology 63 (2004): 1081– 1083.
- H Merle et al. “Treatment of Optic Neuritis by Plasma Exchange (Add-On) in Neuromyelitis Optica,” Ophthalmol 130 (2012): 858.
- R Deschamps et al. “Plasma exchange response in 34 patients with severe optic neuritis,” J Neurol 263 (2016): 883–887.
- N Skorupka et al. “Visual Outcomes of Plasma Exchange Treatment of Steroid- Refractory Optic Neuritis: A Retrospective Monocentric Analysis,” Med. Hemotherapy Off. Organ Dtsch. Ges. Transfusionsmedizin Immunhamatologie 46 (2019): 417–422.
- M Jugnet, T David, M Pierre, et al. “Therapeutic Plasma Exchange for Severe Optic Neuritis in a Region with a High Prevalence of Neuromyelitis Optica,” Ther 14 (2025): 2469–2479.
- S Tan et al. “Vision improvement in severe acute isolated optic neuritis after plasma exchange treatment in Chinese population: a prospective case series study,” Ther Adv Neurol Disord 13 (2020): 1756286420947977.
- K Galetta et al. “Treatment outcomes of first-ever episode of severe optic neuritis,” Mult Scler Relat. Disord 66 (2022): 104020.
- S-H Kim, W Kim, S-Y. Huh, et al. “Clinical efficacy of plasmapheresis in patients with neuromyelitis optica spectrum disorder and effects on circulating anti-aquaporin-4 antibody levels,” J Clin Neurol Seoul Korea 9 (2013): 36–42.
- K-C Wang, S-J Wang, C-L Lee, et al. “The rescue effect of plasma exchange for neuromyelitis optica,” J Clin Neurosci Off J Neurosurg Soc Australas 18 (2011): 43–46.
- Kleiter et al. “Apheresis therapies for NMOSD attacks: A retrospective study of 207 therapeutic interventions,” Neurol Neuroimmunol Neuroinflammation 5 (2018): e504.
- S Thakolwiboon et al. “Outcomes After Acute Plasma Exchange for Myelin Oligodendrocyte Glycoprotein Antibody-Associated Disease,” Neurology 105 (2025): e213903.
- W Song, Y Qu, and X Huang. “Plasma exchange: an effective add-on treatment of optic neuritis in neuromyelitis optica spectrum disorders,” Int Ophthalmol 39 (2019): 2477–2483.
- Z Li et al. “Safety and efficacy of plasma exchange treatment in children with AQP4- IgG positive neuromyelitis optica spectrum disorder,” Immunol 13 (2022): 1113406.


 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 