Novel Transcranial Pulse Stimulation (TPS) in Football-Related Concussion - A Pilot Case Series
Prof. Dr. Karsten Knobloch, FACS1*
SportPraxis Professor Knobloch, Hannover, Germany
*Corresponding Author: Prof. Dr. Karsten Knobloch, SportPraxis Professor Knobloch, Hannover, Germany.
Received: 16 July 2025; Accepted: 23 July 2025; Published: 31 July 2025
Article Information
Citation: Karsten Knobloch. Novel Transcranial Pulse Stimulation (TPS) in Football-Related Concussion - A Pilot Case Series. Journal of Orthopedics and Sports Medicine. 7 (2025): 373-378.
View / Download Pdf Share at FacebookAbstract
Introduction: Concussion has been evolved as a crucial factor especially in collision high-impact sports like Soccer, American Football, Rugby, and Ice hockey. Transcranial pulse stimulation (TPS) is a novel MRI-navigated application of focused electromagnetic extracorporeal shockwave therapy (ESWT) to the brain. In mild to moderate Alzheimer dementia TPS has been shown to significantly improve function and decrease depression symptoms in a clinically significant way. It can improve neuroplasticity in healthy volunteers.
Hypothesis: TPS is feasible and safe in football-related concussion.
Methods: Five male amateur soccer players (25±6yrs) with footballrelated concussion were included in this pilot trial. TPS treatment with Neurolith (Storz Medical Tägerwilen, Suisse) was done on average 48±12 hours after the injury with 6000 shots 0,2mJ/mm2 and in total three TPS sessions every second day. Multiparametric SCAT6 evaluation was done immediately after concussion and at day 7 according to the concussion consensus recommendations.
Results: All five male amateur soccer players tolerated the three TPS session well without any adverse effect. Initial SCAT6 revealed 13±2 symptoms (out of 22) with 24±8 symptom severity (out of 132), orientation 5/5, immediate memory 29/30, concentration 5/5, delayed recall 10/10. Day 7 SCAT6 revealed with 4±3 less symptoms (out of 22) with 9±4 lighter symptom severity (out of 132), orientation 5/5, immediate memory 30/30, concentration 5/5, delayed recall 10/10. Return to play was 7±3days.
Conclusion: In this pilot trial, TPS in football-related concussion was well tolerated and without adverse effects. Return to play was short with 7 days on average. SCAT6 testing revealed a rapid symptom improvement within a week in amateur football players. This pilot observation warrants future larger-scale clinical controlled trials on TPS in football-related concussion.
Keywords
<p>ESWT - extracorporeal shockwave therapy; TPS - Transcranial pulse stimulation; Concussion - return to play – soccer; Soccer; American Football; Rugby; Ice hockey</p>
Article Details
1. Introduction
Concussion has been evolved as a crucial factor especially in collision high-impact sports like Soccer, American Football, Rugby, and Ice hockey. Concussion is a traumatically induced transient disturbance of brain function and involves complex pathophysiological process.
The 2022 consensus statement on concussion in sports define [1]:
"Sport-related concussion is a traumatic brain injury caused by a direct blow to the head, neck or body resulting in an impulsive force being transmitted to the brain that occurs in sports and exercise-related activities. This initiates a neurotransmitter and metabolic cascade, with possible axonal injury, blood flow change and inflammation affecting the brain. Symptoms and signs may present immediately, or evolve over minutes or hours, and commonly resolve within days, but may be prolonged.
No abnormality is seen on standard structural neuroimaging studies (computed tomography or magnetic resonance imaging T1- and T2-weighted images), but in the research setting, abnormalities may be present on functional, blood flow or metabolic imaging studies. Sport-related concussion results in a range of clinical symptoms and signs that may or may not involve loss of consciousness. The clinical symptoms and signs of concussion cannot be explained solely by (but may occur concomitantly with) drug, alcohol, or medication use, other injuries (such as cervical injuries, peripheral vestibular dysfunction) or other comorbidities (such as psychological factors or coexisting medical conditions)."
Animal and human studies support the idea of post-concussive vulnerability, showing that a second blow before the brain has recovered results in worsening metabolic changes within the cell. The concussed brain is less responsive to usual neural activation and when premature cognitive or physical activity occurs before complete recovery the brain may be vulnerable to prolong dysfunction. A history of concussion is associated with a higher risk of sustaining another concussion. Repeated sports-related concussions appear to have a cumulative impact on clinical-but not cognitive-symptom severity [2]. Although clinical symptom burden in athletes with 3+ concussions in the past was not alarmingly high yet, increased caution should be advised at this point. A recent trial revealed an incidence of 5.3 per 1000 athlete exposures at Copa America 2019 tournament [3]. In the lockdown period 2020, the injury rates in US professional men's soccer significantly increased for ACL injuries, muscle injuries and concussions vs. 2018/19 [4].
Three distinct subsets of head injury mechanisms are prevalent in soccer [5]:
- • head-to-equipment
- • head-to-surface
- • head-to-player
Return to play may differ in these regards: those with head-to-equipment/ground injuries spent the shortest time until unrestricted return to play, while those with head-to-ball injuries had the longest time [6]. Notably, a human finite element model revealed that the occiput is most susceptible to brain injuries [7]. In line, soccer ball speeds of 14.0m/s on the occiput differ from 17.2m/s on the frontal head and 17.8m/s on the temporal location. In sports with similar playing rules, the reported incidence of concussion is higher in female than in male athletes. Why female soccer players experience a concussion more often than their male counterparts is still a question of debate [8].
The primary concern of too early return to play is a decreased reaction time leading to an increased risk of repeat concussion or other injury. As such, subclinical concussion has been recently identified as a risk factor for anterior cruciate ligament injury [9].
Chronic traumatic encephalopathy (CTE) is a neurodegenerative disease that has been neuropathologically diagnosed in brain donors exposed to repetitive head impacts, including boxers and American football, soccer, ice hockey, and rugby players like Alzheimer disease. At a microscopic level, the neurons, glia, and blood vessels of the brain are stretched when imperiled by rapid acceleration, deceleration, and rotational forces. More specifically, it is believed that axonal injury, micro-hemorrhage with subsequent loss of blood-brain barrier integrity, and the inflammatory cascade caused by activation of glial cells ultimately results in the deposition of both tau protein and neurofibrillary tangles in specific regions of the brain characteristic of CTE. Thus, CTE is considered a tauopathy along with Alzheimer's disease and other neurodegenerative diseases.
Transcranial pulse stimulation (TPS) is a novel MRI-navigated application of focused electromagnetic extracorporeal shockwave therapy (ESWT) to the brain. In mild to moderate Alzheimer dementia TPS has been shown [10] to significantly improve function and decrease depression symptoms in a clinically significant way. It appears that TPS normalizes the electric activity in EEG in Alzheimer. It can improve neuroplasticity in healthy volunteers. Therefore, given the similarities of the late potential sequelae of repetitive traumatic brain injuries, I developed the following hypothesis: TPS is feasible and safe in football-related concussion.
2. Methods
Five male amateur soccer players (25±6yrs) with football-related concussions were included in this pilot trial.
2.1 Intervention
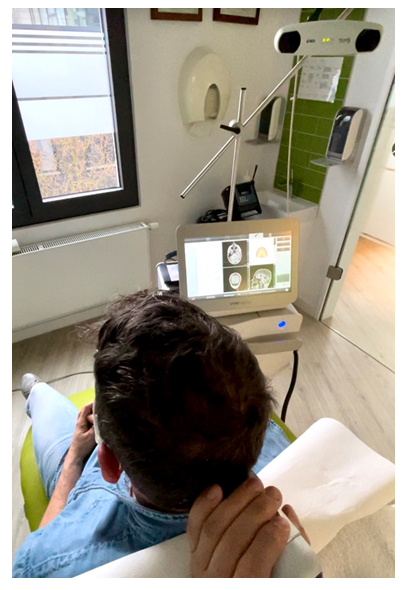
Extracorporeal shockwave therapy (ESWT) is widely used in musculoskeletal disorders of tendons, bones and muscles [11-13]. It is known to act via mechanotransduction and can elicit a protein response depending on the disease state of the tissue treated. Transcranial pulse stimulation (TPS) is an innovative method incorporating electromagnetic generated focused extracorporeal shockwaves (ESWT) with MRI-real time navigation into distinct regions of the brain (Figure 1,2).
The new technique of transcranial pulse stimulation (TPS) may be based on direct stimulation and reactivation of neurons in the brain [14]. Momentum transfer is the basic physical mechanism and the initiator for successive biological processes in medical shock wave therapy.
TPS has been reported to induce neuroplastic changes when stimulated at the left primary somatosensory cortex for more than a week after a single treatment session [15]. In a randomized trial with 60 Alzheimer dementia (AD) patients TPS could significantly improve cognitive scores with an upregulated memory-associated brain activation and functional connectivity in the attention network [16].
The current by far largest report [17] involving 58 patients with Alzheimer's disease (AD) found a clinically relevant improvement of the CERAD score after 10 TPS sessions. In Parkinson's disease, TPS could significantly reduce resting tremor after a single session [18]. A randomized-controlled trial of TPS in attention-deficit/hyperactivity disorder in young adolescents is underway in Hongkong [19].
2.2 TPS treatment parameters
In this pilot trial TPS treatment with Neurolith (Storz Medical Tägerwilen, Suisse) was done on average 48±12 hours after the injury with 6000 shots 0,2mJ/mm2 and in total three TPS sessions every second day (Figure 3).
Patients were seated comfortably and treated over 30minutes.
Since concussion is believed to affect the entire brain given the variety of symptoms, the entire cortex was treated with TPS under MRI-navigation, where color-changes indicate the amount of shots applied in a distinct area.
2.3 Concussion assessment
The Concussion in Sport Group (CISG) integrated measures into one multimodal tool designed to assist clinicians by standardizing an acute assessment across several domains of functioning. The original Sport Concussion Assessment Tool (SCAT) was published in 2005 [20] and contained educational information, a concussion symptoms scale and information on management of concussion. In the years that followed several iterations of the SCAT have been published, informed by empirical data, systematic reviews and clinical experience. Each iteration of the SCAT evolved along with the scientific literature, with each version increasingly representing the complexity and multimodal nature of SRC assessment [21].
As far as SCAT6 is concerned, the following considerations are worthwhile:
- • The SCAT is most effective in discriminating between concussed and non-concussed athletes up to 7 days postinjury, with diminishing clinical utility after 72 hours. It is suggested that if the time frame is greater than 7 days after injury, the SCOAT6/Child SCOAT6 should be considered.
- • The SCAT6 is for use with adolescents (>12 years), and adults. The Child SCAT6 is for use with children aged 8-12.
- • The SCAT6 is intended to be an aide in the standardized evaluation of SRC during the acute phase of injury. It is not intended to be used as a stand-alone diagnostic tool but rather to inform clinical assessment and diagnosis.
- • It is important to underscore that ‘concussed’ athletes may perform within normal ranges on the SCAT6 (false negative) just as ‘normal’ individuals may perform poorly (false positive).
- • Interpretation of SCAT6 data is a clinical endeavor that includes examining the athlete in the context of personal, psychological, social, cultural, athletic, medical, injury characteristics/mechanism and educational history/factors.
- • Clinicians must familiarize themselves with best practices in the administration of standardized tests, use of appropriate normative data, interpretation of postinjury scores, psychometric test properties and the proper analysis of multiple tests used simultaneously (eg, population base rates) when using the SCAT6.
- • Clinicians who choose to use baseline data must familiarize themselves with reliable change metrics and base rates of reliable change scores.
- • Baseline testing may be useful when resources (eg, financial, personnel, time) permit, such as at the professional or elite level, but the evidence does not support compulsory use at other levels of sport, such as at the child and adolescent level.
- • When a baseline assessment is given, test users should be familiar with identification of performance invalidity on the SCAT6.
- • Performance well below emerging normative standards should trigger repeat and/or additional cognitive evaluation to establish an accurate baseline and/or rule out true cognitive impairment.
- • The SCAT6 is not intended to be used in isolation for making return-to-sport decisions.
Multiparametric SCAT6 evaluation was done immediately after concussion and at day 7 according to the concussion consensus recommendations.
3. Results
3.1 Adverse effects
All five male amateur soccer players tolerated the three TPS session well without any adverse effect.
3.2 Baseline SCAT6 assessments
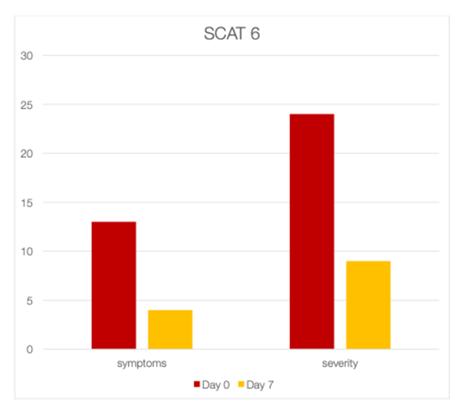
Initial SCAT6 revealed 13±2 symptoms (out of 22) with 24±8 symptom severity (out of 132), orientation 5/5, immediate memory 29/30, concentration 5/5, delayed recall 10/10 (Figure 4).
3.3 Day 7 SCAT 6 assessments
Day 7 SCAT6 revealed with 4±3 less symptoms (out of 22) with 9±4 lighter symptom severity (out of 132), orientation 5/5, immediate memory 30/30, concentration 5/5, delayed recall 10/10.
3.4 Return to play after concussion with TPS
Return to play was 7±3days.
4. Discussion
This pilot report demonstrates the safety and feasibility of transcranial pulse stimulation (TPS), which is MRI-navigated focused electromagnetic extracorporeal shockwave therapy (ESWT) to the brain in soccer players with concussion. Both the number of symptoms as well as the severity of symptoms assessed by the validated SCAT6 assessment tool are significantly reduced within a week after three TPS sessions. While being a pilot case series in concussion, further larger-scale controlled trials are mandatory to elucidate the role of TPS in concussion in collision sports preferably.
4.1 Return to play
The UEFA Elite Club Injury Study [22] reports an 8.7days (6,6-10,8) time loss following a concussion in professional soccer. In this pilot case series, we found a return to play of 7±3days with three TPS sessions starting on average 48hours after the concussion. It is tempted to speculate that an even earlier or immediate start after the concussion and potentially more sessions than three TPS session as in this pilot report might further improve the SCAT6 assessments and potentially shorten the return to play time even more.
Consensus is that concussion symptoms should be resolved before returning to exercise again. A gradual, stepwise increase in physical demands and loaded is recommended. An aerobic exercise has been recently found to be feasible and tolerable via stationary cycling in the post-acute (14-25 days post-injury) phase of concussion in a RCT [23]. Transitory kinesiophobia may be evident within 14 days after injury using Tampa scale of kinesiophobia following concussion [24]. Notably, in hockey player with a history of concussions heart rate variability as a marker for cardio-autonomic function showed a significant higher standard deviation of NN intervals indicating cardio-autonomic dysfunction [25]. Furthermore, speech rate in concussed athletes aged 19-22yrs is slower with longer average time per syllable needing more speech muscle activation than controls [26].
A recent exploratory study [27] among retired male soccer players reveled neurophysiological changes measured with transcranial magnetic stimulation (TMS). TPS has been studied extensively in Alzheimer dementia demonstrating significant improvement in the functional connectivity of key brain regions correlated with cognitive improvement [28]. These results have been replicated by others [29,30].
5. Conclusions
In this pilot trial, TPS in football-related concussion was well tolerated and without adverse effects. Return to play was short with 7 days on average. SCAT6 testing revealed a rapid symptom improvement within a week in amateur football players. This pilot observation warrants future larger-scale clinical controlled trials on TPS in football-related concussion.
Ethics Approval and Informed Consent
All patients were informed that data from the cases would be submitted for publication and gave consent.
Funding
There is no funding to report.
Disclosure
KK is a lecturer for Storz Medical.
References
- Patricios JS, Schneider KJ, Dvorak J, et al. Consensus statement on concussion in sport: the 6th international conference on concussion in sport-Amsterdam Br J Sports Med 57 (2023): 695-711.
- Glaser J, Jaeckle S, Beblo T, et al. The effect of repeated concussions on clinical and neurocognitive symptom severity in different contact sports. Scand J Med Sci Sports 34 (2024): e14626.
- Pangrazio O, Forriol F, Aguirre AS, et al. Enhancing protocols for concussion management in professional soccer events. Cureus 16 (2024): e64064.
- Hardin S, Silverman R, Brophy R, et al. Epidemiology of injury and illness in North American Professional men's soccer: comparing COVID-19 lockdown with previous seasons. Sports Health 18 (2024): 19417381241253227.
- Jordan L, Andrie J. Concussions in soccer. Sports Med Arthrosc Rev 32 (2024): 125-130.
- Jo J, Boltz AJ, Williams KL et al. Mechanisms of injury leading to concussions in collegiate soccer players: A CARE consortium study. Am J Sports Med 52 (2024): 1585-1595.
- Cao Y, Liu Y, Tang L, et al. Quantitative assessment of brain injury and concussion induced by an unintentional soccer ball impact. Injury 55 (2024): 111658.
- Blyth RJ, Alcock M, Tumilty DS. Why are female soccer players experiencing a concussion more often than their male counterparts? A scoping review. Phys Ther Sport 52 (2021): 54-68.
- Kakavas G, Malliaropoulos N, Blach W, et al. Ball heading and subclinical concussion in soccer as a risk factor for anterior cruciate ligament injury. J Orthop Surg Res 16 (2021): 566.
- Beisteiner R, Matt E, Fan C, et al. Transcranial pulse stimulation with ultrasound in Alzheimer’s disease-a new navigated focal brain therapy. Adv Sci (Weinh) 7 (2021): 1902583.
- Mani-Babu S, Morrissey D, Waugh C, et al. The effectiveness of extracorporeal shock wave therapy in lower limb tendinopathy: a systematic review. Am J Sports Med 43 (2015): 752-61.
- Korakakis V, Whiteley R, Tzavara A, et al. The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: a systematic review including quantification of patient-rated pain reduction. Br J Sports Med 52 (2018): 387-407.
- Rhim HC, Shin J, Kang J, et al. Use of extracorporeal shockwave therapies for athletes and physically active individuals: a systematic review. Br J Sports Med 58 (2024): 154-163.
- Wess O, Mayer J. The interaction of shock waves with biological tissue-momentum trasnfer, the key for tissue stimulation and fragmentation. Int J Surg (2025).
- Matt E, Kaindl L, Tenk S, et al. First evidence of long-term effects of transcranial pulse stimulation (TPS) on the human brain. J Transl Med 20 (2022): 26.
- Matt E, Metterwallner M, Radjenovic S, et al. Ultrasound neuromodulation with transcranial pulse stimulation in Alzheimer disease. JAMA Netw Open 8 (2025): e2459170.
- Radjenovic S, Bender L, Gaal M, et al. A retrospective analysis of ultrasound neuromodulation therapy using transcranial pulse stimulation in 58 dementia patients. Pyschol Med 55 (2025): e70.
- Manganotti P, Liccari M, Lombardo TMI, et al. Effect of s single session of transcranial pulse stimulation (TPS) on resting tremor in patients with Parkinson's disease. Brain Res 1850 (2025): 149405.
- Cheung T, Yee BK, Chau B. Efficacy and safety of transcranial pulse stimulation in young adolescents with attention-deficit/hyperactivity disorder: a pilot, randomized, double-blind, sham-controlled trial. Fron Neurol 15 (2024): 1364270.
- McCrory P. Summary and agreement statement of the 2nd international conference on concussion in sport, Prague BJSM 39 (2003): 78-86.
- Echemendia RJ, Brett BL, Broglio S, et al. Introducing the sport concussion assessment tool 6 (SCAT6). Br J Sports Med 57 (2023): 615-616.
- Ekstrand J, Krutsch W, Spreco A, et al. Time before return to play for the most common injuries in professional football: a 16-year follow-up of the UEFA Elite Club Injury Study. Br J Sports Med 54 (2020): 421-426.
- Snyder AR, Greif SM, Clugston JR, et al. The effect of aerobic exercise on concussion recovery: a pilot clinical trial. J Int Neuropsychol Soc 27 (2021): 790-84.
- Reinking S, Seehusen CN, Walker GA, et al. Transitory kinesiophobia after sport-related concussion and its correlation with reaction time. J Sci Med Sport 29 (2021): S1440-2440.
- Harrison AT, Lane-Cordova A, La Fountaine MF, et al. Impact of concussion history on heart rate variability during bouts of acute stress. J Athl Train 20 (2021).
- Banks RE, Beal DS, Hunter EJ. Sports related concussion impacts speech rate and muscle physiology. Brain Inj 9 (2021): 1-9.
- Pearce AJ, Tallent J, Frazer AK, et al. The effect of playing career on chronic neurophysiologic changes in retired male football players: an exploratory study using transcranial magnetic stimulation. J Clin Neurophysiol (2025).
- Lo HKY, Fong TKH, Cheung T, et al. Enhanced cognition and modulation of brain connectivity in mild neurocognitive disorder: the promise of transcranial pulse stimulation. Biomedicines 12 (2024): 2081.
- Shinzato GT, Assone T, Sandler PC, et al. Non-invasive sound wave brain stimulation with transcranial pulse stimulation (TPS) improves neuropsychiatric symptoms in Alzheimer's disease. Brain Stimul 17 (2024): 413-415.
- Chen X, You J, Ma H, et al. Transcranial pulse stimulation in Alzheimer's disease. CNS Neurosci Ther 30 (2023): e14372.




 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 